Authors
Yan Wang, Ziyuan Zhou, Luomengjia Dai, Yiwen Hua, Yujie Wu, Rong Wang, Lei Fan, Jianyong Li, Juejin Wang, Huayuan Zhu.
Background
Real-time monitoring is essential for the management of chronic lymphocytic leukemia (CLL) patients. Peripheral blood analysis offers advantages of affordability, convenience, and suitability for longitudinal disease tracking. However, current blood film evaluation methods lack automation and are subject to observer bias, affecting reproducibility and clinical translation. Moreover, CLL exhibits complex morphological and biological heterogeneity, with subtle cellular changes potentially heralding disease progression or transformation. To address these unmet needs, we developed an AI-driven system for objective, high-throughput evaluation of peripheral blood cell morphology in CLL.
Methods
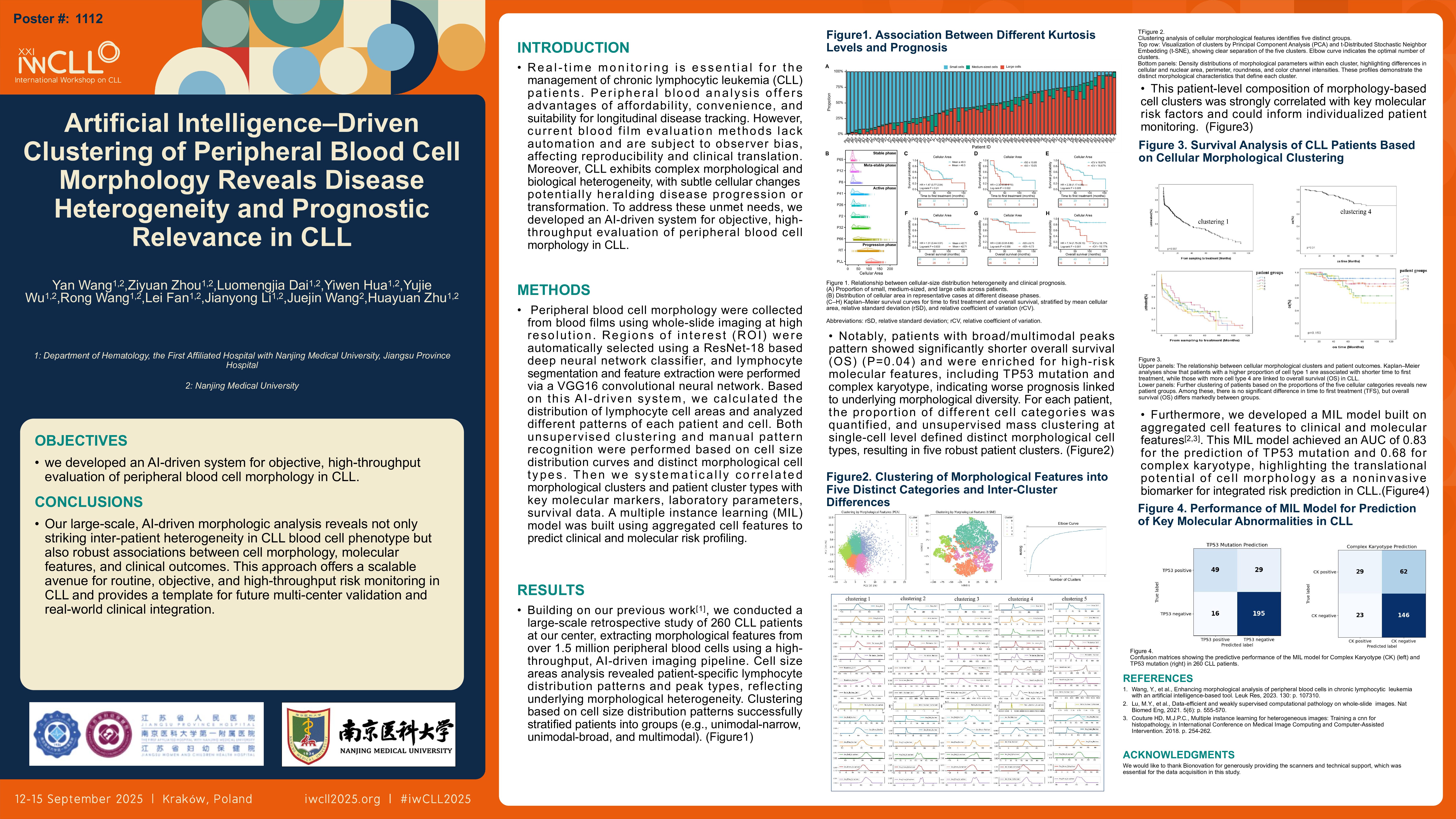
Peripheral blood cell morphology were collected from blood films using whole-slide imaging at high resolution. Regions of interest (ROI) were automatically selected using a ResNet-18 based deep neural network classifier, and lymphocyte segmentation and feature extraction were performed via a VGG16 convolutional neural network. Based on this AI-driven system, we calculated the distribution of lymphocyte cell areas and analyzed different patterns of each patient and cell. Both unsupervised clustering and manual pattern recognition were performed based on cell size distribution curves and distinct morphological cell types. Then we systematically correlated morphological clusters and patient cluster types with key molecular markers, laboratory parameters, survival data. A multiple instance learning (MIL) model was built using aggregated cell features to predict clinical and molecular risk profiling.
Results
Building on our previous work, we conducted a large-scale retrospective study of 260 CLL patients at our center, extracting morphological features from over 1.5 million peripheral blood cells using a high-throughput, AI-driven imaging pipeline. Cell size areas analysis revealed patient-specific lymphocyte distribution patterns and peak types, reflecting underlying morphological heterogeneity. Clustering based on cell size distribution patterns successfully stratified patients into groups (e.g., unimodal-narrow, unimodal-broad, and multimodal). Notably, patients with broad/multimodal peaks pattern showed significantly shorter overall survival (OS) (P=0.04) and were enriched for high-risk molecular features, including TP53 mutation and complex karyotype, indicating worse prognosis linked to underlying morphological diversity. For each patient, the proportion of different cell categories was quantified, and unsupervised mass clustering at single-cell level defined distinct morphological cell types, resulting in five robust patient clusters. This patient-level composition of morphology-based cell clusters was strongly correlated with key molecular risk factors and could inform individualized patient monitoring. Furthermore, we developed a MIL model built on aggregated cell features to clinical and molecular features. This MIL model achieved an AUC of 0.83 for the prediction of TP53 mutation and 0.68 for complex karyotype, highlighting the translational potential of cell morphology as a noninvasive biomarker for integrated risk prediction in CLL.
Conclusion
Our large-scale, AI-driven morphologic analysis reveals not only striking inter-patient heterogeneity in CLL blood cell phenotype but also robust associations between cell morphology, molecular features, and clinical outcomes. This approach offers a scalable avenue for routine, objective, and high-throughput risk monitoring in CLL and provides a template for future multi-center validation and real-world clinical integration.
Keywords : Artificial Intelligence, Peripheral Blood Cell Morphology, Chronic Lymphocytic Leukemia
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: