Authors
Yi Miao, Chun Qiao, Huimin Jin, Lei Fan, Jianyong Li
Introduction
In chronic lymphocytic leukemia (CLL), SF3B1 mutations, identified in approximately 10–15% of cases, are recognized as potential driver mutations. SF3B1 mutations have been reported to predict worse outcomes in patients with CLL. While the majority of SF3B1-mutated CLL cases harbored SF3B1 K700E, the clinical significance of other SF3B1 variants remain less well-studied. This study aimed to investigate the clinical significance of specific SF3B1 mutation variants in Chineses patients with CLL.
Methods
A total of 531 cases of CLL from the First Affiliated Hospital of Nanjing Medical University (Jiangsu Province Hospital) were included in this study. Clinical data were collected. Targeted sequencing was performed on fresh bone marrow aspirate or peripheral blood samples with sufficient tumor cells. Genomic DNA (gDNA) was used to generate sequencing libraries using the MultipSeq Custom Panel (Rightongene Biotechnology Co. Ltd., Shanghai, China) following the manufacturer’s protocols. Sequencing was performed on the MiSeq/Novaseq (Illumina, United States) platform. Overall survival (OS) was defined as time from diagnosis to death from any cause or last follow-up. Time to the fisrt treatment (TTFT) was defined as time from diagnosis to the first treatment or last known untreated date.
Results
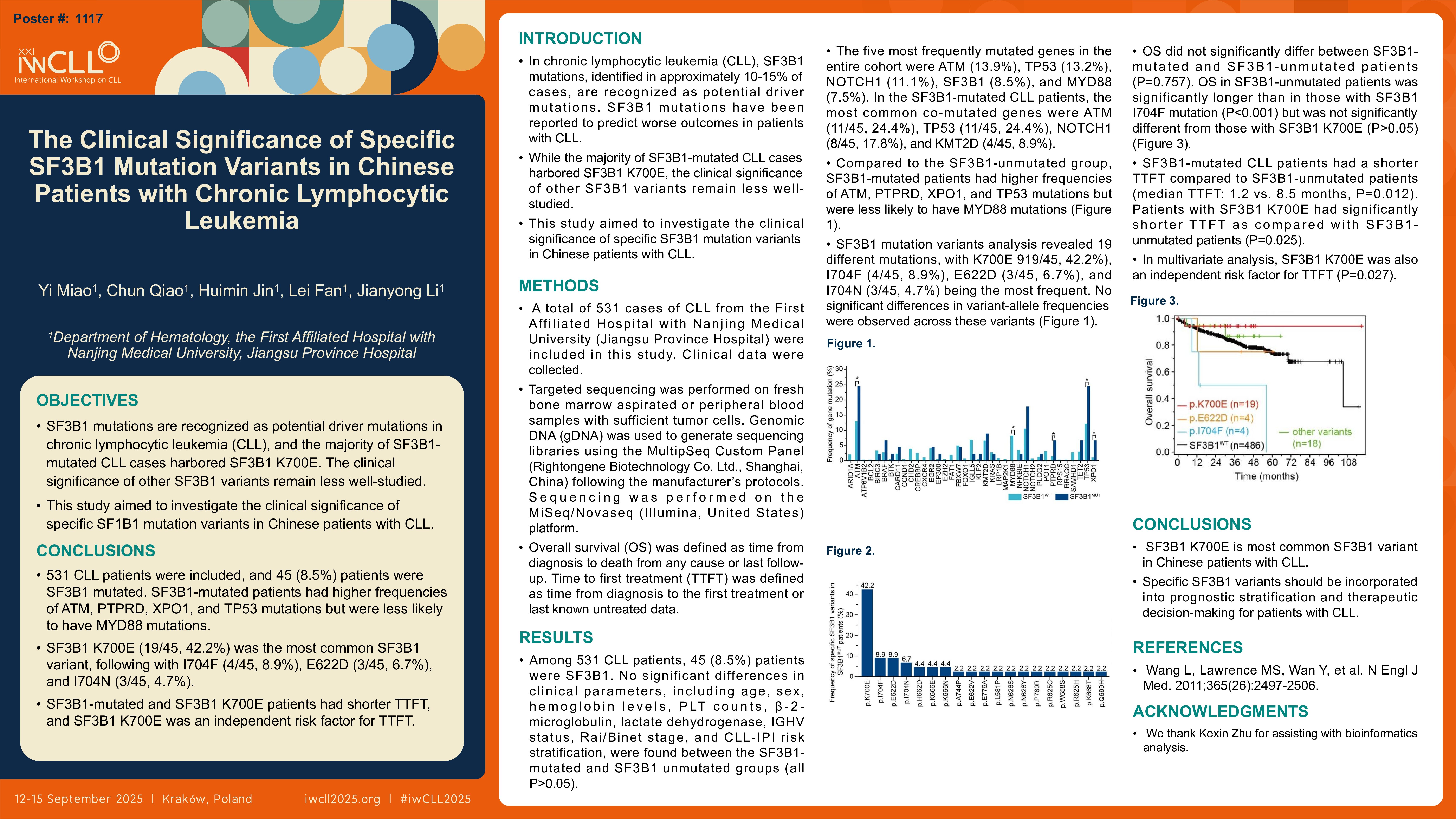
Among 531 CLL patients, 45 (8.5%) patients were SF3B1 mutated. No significant differences in clinical parameters, including age, sex, hemoglobin levels, PLT counts, β-2-microglobulin, lactate dehydrogenase, IGHV status, Rai/Binet stage, and CLL-IPI risk stratification, were found between the SF3B1-mutated and SF3B1-unmutated groups (all P>0.05). The five most frequently mutated genes in the entire cohort were ATM (13.9%), TP53 (13.2%), NOTCH1 (11.1%), SF3B1 (8.5%), and MYD88 (7.5%). In the SF3B1-mutated CLL patients, the most common co-mutated genes were ATM (11/45, 24.4%), TP53 (11/45, 24.4%), NOTCH1 (8/45, 17.8%), and KMT2D (4/45, 8.9%). Compared to the SF3B1-unmutated group, SF3B1-mutated patients had higher frequencies of ATM, PTPRD, XPO1, and TP53 mutations (P=0.042, P=0.045, P=0.024, and P=0.034, respectively) but were less likely to have MYD88 mutations (P=0.039). SF3B1 mutation variants analysis revealed 19 different mutations, with K700E (19/45, 42.2%), I704F (4/45, 8.9%), E622D (3/45, 6.7%), and I704N (3/45, 6.7%) being the most frequent. No significant differences in variant-allele frequencies were observed across these variants. OS did not significantly differ between SF3B1-mutated and SF3B1-unmutated patients (P=0.757). SF3B1-mutated CLL patients had a shorter TTFT compared to SF3B1-unmutated patients (median TTFT: 1.2 vs. 8.5 months, P=0.012). OS in SF3B1-unmutated patients was significantly longer than in those with SF3B1 I704F mutation (P < 0.001) but was not significantly different from those with SF3B1 K700E (P>0.05). Patients with SF3B1 K700E had significantly shorter TTFT as compared with SF3B1-unmutated patients (P=0.025). In multivariate analysis, SF3B1 K700E was also an independent risk factor for TTFT (P=0.027).
Conclusion
SF3B1 K700E is most common SF3B1 variant in Chinese patients with CLL. Specific SF3B1 variants should be incorporated into prognostic stratification and therapeutic decision-making for patients with CLL.
Keywords : chronic lymphocytic leukemia, SF3B1, variants
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: