Authors
Samir Mouhssine, Chiara Cosentino, Mohammad Almasri, Nawar Maher, Jana Nabki, Luca Cividini, Bashar, Al Deeban, Milena Lazzaro, Francesca Maiellaro, Riccardo Dondolin, Matteo Bellia, Eleonora Secomandi, Valeria Caneparo, Abdurraouf Mahmoud, Clara Deambrogi, Sreekar Kogila, Jospeh Ghanej, Silvia Rasi, Gianluca Gaidano, Riccardo Moia.
Background
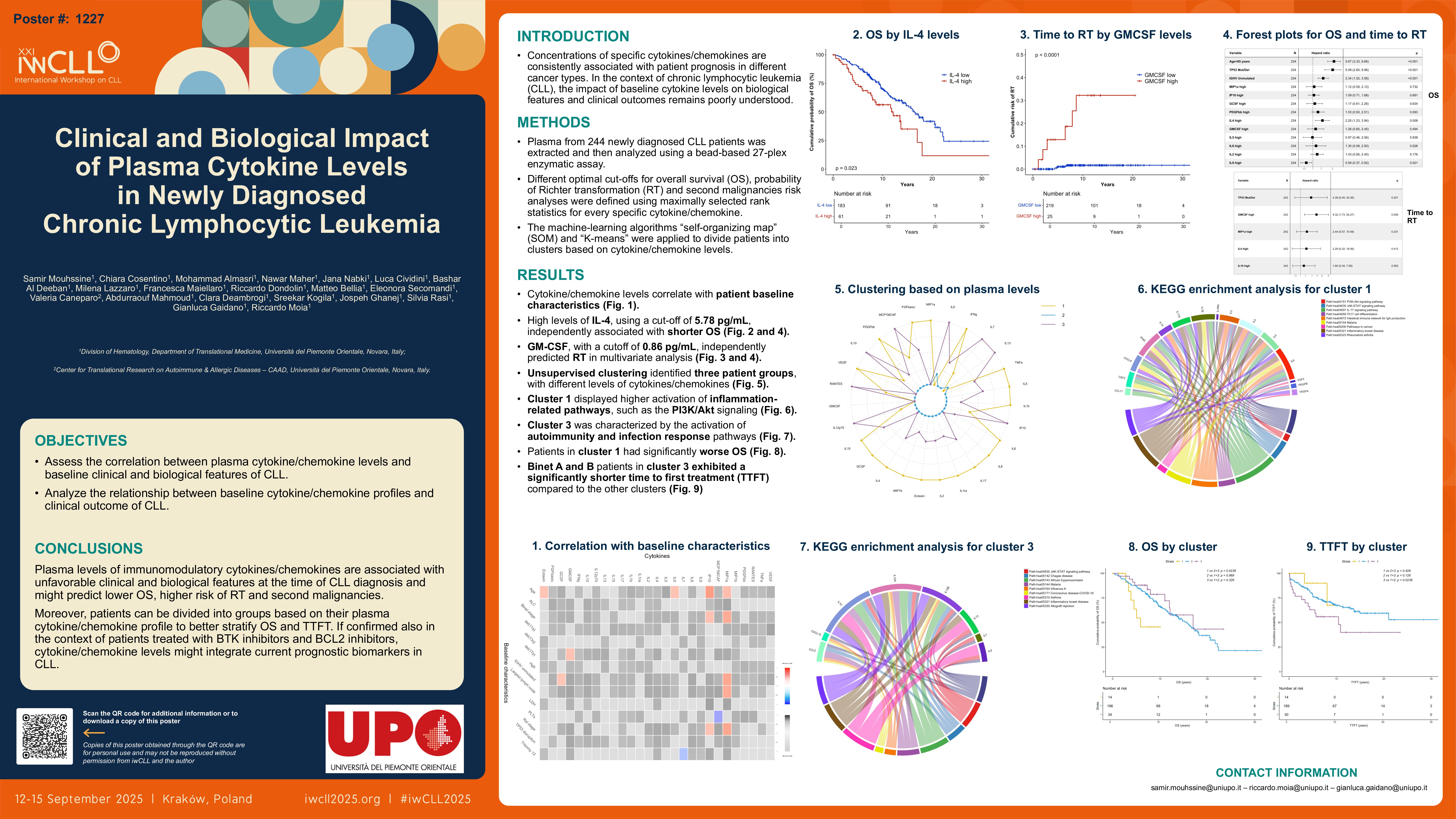
Concentrations of specific cytokines/chemokines are consistently associated with patient prognosis in different cancer types (Lippitz, Lancet Oncol. 2013). In the context of chronic lymphocytic leukemia (CLL), the impact of baseline cytokine levels on biological features and clinical outcomes remains poorly understood. Previous findings have suggested a prognostic role for MIP-1α in predicting unfavorable clinical and biological characteristics (Sivina et al., Blood. 2011). However, little is known about the role of other cytokines/chemokines in CLL.
Methods
Plasma from newly diagnosed CLL patients was analyzed for cytokine/chemokine levels using the Bio-Plex Pro Human Cytokine 27-plex assay (BioRad). Associations with baseline clinical and biological features were assessed via Mann-Whitney U test and Spearman correlation. Survival analyses were performed through the Kaplan-Meier and log-rank tests. Different optimal cut-offs for overall survival (OS), probability of Richter transformation (RT) and second malignancies risk analyses were defined using maximally selected rank statistics (maxstat package). For each clinical outcome, patients with cytokine/chemokine concentrations above the optimal cutoff for every specific cytokine/chemokine were marked as “high”, while those below were marked as “low”. P-values were adjusted using the Benjamini-Hochberg correction.
Results
A total of 244 patients with newly diagnosed CLL were included. Median age at diagnosis was 68.9 years; 73 patients (29.9%) had unmutated immunoglobulin heavy chain variable region (IGHV) genes, and 16 (6.6%) had TP53 disruption. After a median follow-up of 13.4 years, the median OS was 15.7 years. By correlating cytokines/chemokines with patient baseline clinical and molecular features, elevated MIP-1α levels were significantly associated with unmutated IGHV genes (p < 0.0001), greater lymph node diameter (p < 0.0001), and advanced Rai and Binet stages (both p< 0.0001). Higher IP-10 levels significantly associated with advanced Rai (p=0.02) and Binet (p=0.01) stages. High levels of G-CSF correlated with unmutated IGHV (p=0.049), and elevated GM-CSF levels were associated with del(17p) (p=0.03). Increased MCP-1 was linked to lower platelet count (p < 0.0001).
At diagnosis, multiple cytokines/chemokines with levels exceeding the optimal cut-offs for predicting OS, namely MIP-1α (p= 0.001), IP-10 (p= 0.003), G-CSF (p= 0.011), PDGF-BB (p= 0.023), IL-4 (p=0.023), GM-CSF (p=0.025), IL-5 (p=0.025), IL-6 (p=0.027), and IL-2 (p=0.027) were significantly associated with shorter survival. In multivariate analysis (adjusted for age, IGHV, and TP53 status), high levels of IL-4, using a cut-off of 5.78 pg/mL, independently associated with shorter OS (HR 2.2, p=0.008). Pathway gene enrichment analysis revealed that cytokines/chemokines predicting shorter OS are involved in key molecular pathways regulating cell proliferation, survival, and apoptosis. In particular, G-CSF, GM-CSF, IL-2, IL-4, IL-5, IL-6, and PDGF-BB clustered in the JAK-STAT signaling pathway (fold enrichment 109.9, p=2.23E-12), whereas G-CSF, IL-2, IL-4, IL-6, and PDGF-BB clustered in the PI3K-Akt pathway (fold enrichment 35.9, p=9.17E-07). Regarding RT, high levels of GM-CSF (p < 0.0001), MIP1-α (p=0.034), IL-4 (p=0.034), and IL-10 (p=0.034) were significantly associated with increased risk of RT in univariate analysis. GM-CSF, with a cutoff of 0.86 pg/mL, independently predicted RT in multivariate analysis (HR 9.32, p=0.009). Moreover, among patients who developed a second malignancy after CLL diagnosis, high levels of MIP-1β (p=0.0001), RANTES (p=0.023), and MIP-1α (p=0.023), were linked to shorter time of cancer occurrence. MIP-1β, using a cutoff of 255.36 pg/mL, retained an independent prognostic value for shorter time to second cancer in multivariate analysis also including prior chemo-immunotherapy exposure for CLL (HR 4.64, p=0.002).
Conclusions
Plasma levels of immunomodulatory cytokines/chemokines are associated with unfavorable clinical and biological features at the time of CLL diagnosis. Moreover, higher concentrations of immunomodulatory cytokines/chemokines correlate with lower OS, higher risk of RT and second malignancies. If confirmed also in the context of patients treated with BTK inhibitors and BCL2 inhibitors, cytokine/chemokine levels might integrate current prognostic biomarkers in CLL.
Keywords : chronic lymphocytic leukemia, cytokines, biomarker
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: