Authors
Nadia Bertola, Fabiana Ferrero, Vanessa Cossu, Ennio Nano, Monica Colombo, Rosanna Massara, Maria Cristina Capra, Adalberto Ibatici, Emanuele Angelucci, Fortunato Morabito, Franco Fais, Manlio Ferrarini, Silvia Ravera, Giovanna Cutrona.
Chronic Lymphocytic Leukemia (CLL) is a malignancy of mature B cells, characterized by the clonal accumulation of CD5⁺ CD19+ lymphocytes in blood, bone marrow, and lymphoid tissues (Chiorazzi et al, N Engl J Med, 2005). Despite the significant clinical advances brought by targeted therapies, such as B-cell receptor (BCR) and BCL2 inhibitors, the disease remains incurable and relapse is common (Hallek et al, Lancet, 2018; Hallek et al, Blood, 2018). It is now well established that the CLL microenvironment plays a pivotal role in sustaining leukemic cell survival, contributing to drug resistance through both direct contact with accessory cells and cytokine-mediated signaling. Among these, IL-23 has emerged as a key player. Leukemic cells can express a functional IL-23 receptor (IL-23R) complex and produce IL-23 upon activation, creating an autocrine/paracrine loop that promotes clonal selection and proliferation, independent of BCR signaling (Cutrona et al, Sci Transl Med., 2018). This mechanism may contribute to the persistence of minimal residual disease under targeted treatment. Given the shared structural features of IL-12 family cytokines (IL-12, IL-23, and IL-35) and the overlapping components of their receptor subunits, we hypothesized that these cytokines could differentially influence CLL cell behavior, particularly at the metabolic level, potentially uncovering novel vulnerabilities.
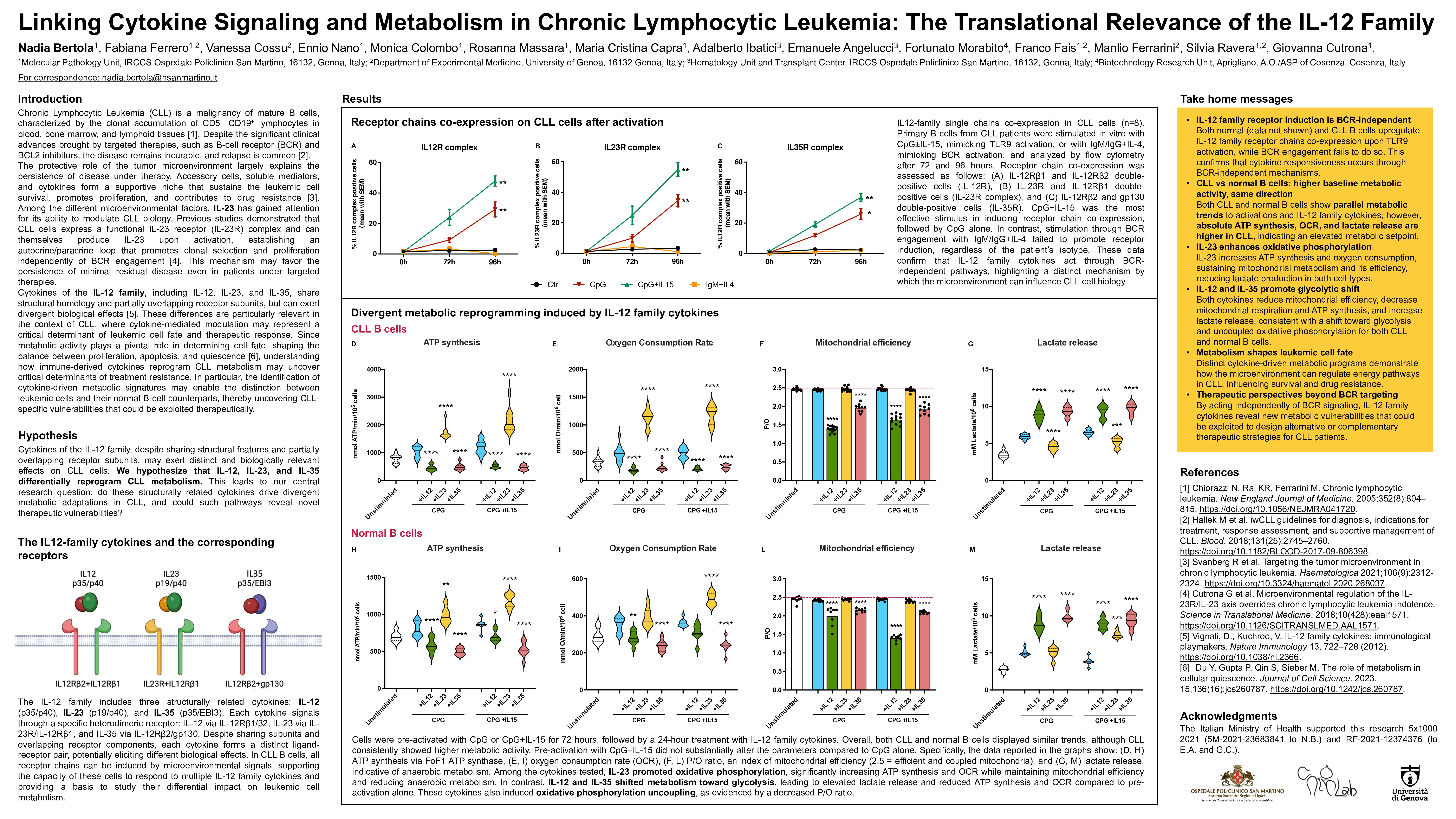
To investigate this, B cells from CLL patients and age-matched healthy donors were stimulated in vitro with a TLR9 agonist (CpG-ODN), mimicking a BCR-independent microenvironmental activation. Expression of IL-12 family receptor chains (IL-12Rβ1, IL-12Rβ2, IL-23R, gp130, and WSX-1) was evaluated by flow cytometry. We then examined the metabolic consequences of stimulation with IL-12, IL-23, and IL-35 by assessing mitochondrial respiration, glycolysis, and ATP production through oximetric, luminometric, and spectrophotometric assays. All analyses were performed under protocols that were ethically approved (CER-Liguria-ID 10115) and in accordance with the Declaration of Helsinki, with informed consent obtained from all participants.
Our results show that all receptor chains for IL-12 family cytokines can be induced in both CLL and normal B cells following TLR9 stimulation, indicating potential responsiveness to IL-12, IL-23, and IL-35. Metabolically, only IL23 maintained or enhanced mitochondrial function in CLL cells, supporting oxidative phosphorylation and ATP-linked respiration. In contrast, exposure to IL-12 and IL-35 led to a decline in mitochondrial efficiency and a shift toward glycolysis, suggestive of metabolic stress or adaptation. Notably, these cytokine effects were more pronounced in leukemic cells than in their normal counterparts, indicating disease-specific metabolic vulnerabilities.
These findings reveal that structurally related cytokines can exert functionally opposite effects on CLL cells’ metabolism and survival. While IL-23 promotes energy-efficient metabolism and favors leukemic persistence, IL-12 and IL-35 impair mitochondrial function, potentially sensitizing cells to metabolic stress or additional therapeutic interventions. The differential impact of IL-12 family members on leukemic metabolism may help explain the incomplete responses observed with current targeted therapies and opens new avenues for therapeutic modulation of the microenvironment. Inhibiting the IL-23/IL-23R axis or harnessing the anti-survival effects of IL-12 and IL-35 may represent promising strategies to overcome resistance and improve long-term disease control in CLL.
Keywords : Chronic Lymphocytic Leukemia, IL-12 Family, Microenvironment, Mitochondrial Metabolism
Please indicate how this research was funded. : This study was supported by the Italian Ministry of Health: 5×1000 2021 (5M-2021-23683841 to N.B.) and RF-2021-12374376 (to E.A. and G.C.).
Please indicate the name of the funding organization.: Italian Ministry of Health