Authors
Mazyar Shadman, Talha Munir, Shuo Ma, Masa Lasica, Monica Tani, Tadeusz Robak, Ian W. Flinn, Jennifer R. Brown, Paolo Ghia, Emmanuelle Ferrant, Constantine S. Tam, Wojciech Janowski, Wojciech Jurczak, Linlin Xu, Tian Tian, Stephanie Agresti, Jamie Hirata, Alessandra Tedeschi.
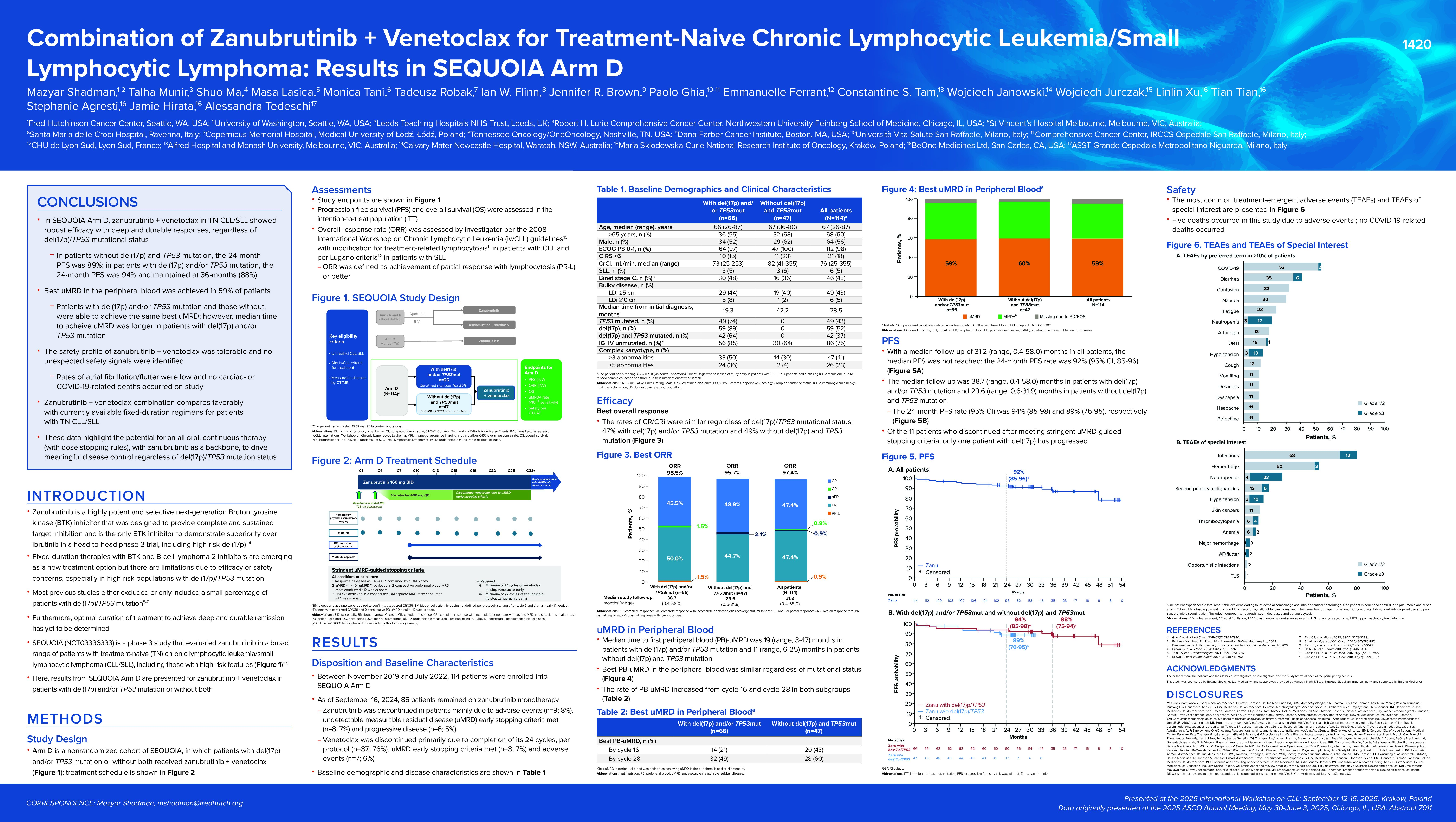
Background
Zanubrutinib monotherapy demonstrated superior progression-free survival (PFS) compared with bendamustine + rituximab in patients without del(17p) at 26.2-month follow-up and sustained PFS benefit at 5-year follow-up. In a single-arm cohort, zanubrutinib monotherapy was also shown to be effective in patients with del(17p). Several chronic lymphocytic leukemia (CLL) studies have demonstrated promising efficacy with the combination of B-cell lymphoma 2 + Bruton tyrosine kinase inhibitors; however, patients with del(17p)/TP53 mutation comprised a small percentage of or were excluded from study populations. Here, we present results from SEQUOIA (NCT03336333) arm D with zanubrutinib + venetoclax in patients with or without del(17p) and/or TP53 mutation.
Methods
Arm D is a nonrandomized cohort of the SEQUOIA study in patients aged ≥65 years (or 18-64 years with comorbidities). Patients received zanubrutinib (160 mg twice daily) + venetoclax (ramp-up to 400 mg once daily) from cycle 4 to cycle 28, followed by continuous zanubrutinib monotherapy until progressive disease, unacceptable toxicity, or meeting undetectable minimal residual disease (uMRD)–guided early zanubrutinib or venetoclax stopping rules (complete response/complete response with incomplete hematologic recovery rate [CR/CRi] and uMRD [ < 1×10−4 by flow cytometry] in peripheral blood and bone marrow on two consecutive tests ≥12 weeks apart). Efficacy responses were assessed by investigator every 3 cycles until cycle 28, then every 6 cycles with peripheral blood minimal residual disease assessment.
Results
Between Nov 2019-Jul 2022, 114 patients were enrolled: 66 (58%) with del(17p) and/or TP53 mutation, 47 (41%) without del(17p) and TP53 mutation, and 1 with missing TP53 results. In all patients, median age was 67 years (range, 26-87), 64 (56%) were male, 86 (75%) had unmutated IGHV, and 47 (41%) had complex karyotype (≥3 abnormalities). As of Sept 16, 2024, the median study follow up was 31 months; 85 (75%) patients remained on zanubrutinib treatment and all patients had discontinued or completed venetoclax treatment. The most common reasons for early discontinuation were reaching the uMRD-guided early stopping rules (zanubrutinib: 7%; venetoclax: 7%), adverse events (zanubrutinib: 8%; venetoclax: 6%), and progressive disease (zanubrutinib: 5%; venetoclax: 4%). Six patients died (5 due to non–treatment-related adverse events and 1 due to progressive disease). In the total population, the 24-month PFS rate was 92%. For patients with del(17p) and/or TP53 mutation, the 24-month PFS rate was 94% and for patients without del(17p) and TP53 mutation, 24-month PFS rate was 89%. The best peripheral blood uMRD rate was 59% in the total population and 59% and 60% in patients with del(17p) and/or TP53 mutation and without del(17p) and TP53 mutation, respectively. Median time to first peripheral blood uMRD was 19 months (range, 3-47) in patients with del(17p) and/or TP53 mutation and 11 months (6-25) in patients del(17p) and TP53 mutation. There were 112 patients with at least one evaluable efficacy assessment. For evaluable patients, the overall response rate and CR/CRi rate was 99% and 49%, in the total population, 100% and 48% in patients with del(17p) and/or TP53 mutation, and 98% and 50% in patients without del(17p) and TP53 mutation. The most common any-grade treatment-emergent adverse events (TEAEs) in all patients were COVID-19 (54%), diarrhea (41%) contusion (32%), and nausea (30%). The most common grade ≥3 TEAEs were neutropenia (17%), hypertension (10%), diarrhea (6%), and neutrophil count decreased (6%).
Conclusions
SEQUOIA arm D data demonstrate promising efficacy and tolerability of zanubrutinib + venetoclax combination treatment in treatment-naive CLL/SLL, regardless of del(17p) and/or TP53 mutational status. Best peripheral blood uMRD was also similar regardless of mutational status. The safety profile of zanubrutinib + venetoclax was consistent with results of prior zanubrutinib studies, and no new safety signals were identified. These data suggest that zanubrutinib plus venetoclax is a promising treatment option for patients with treatment-naive CLL/SLL, regardless of the presence of del(17p) and/or TP53 mutations. Updated data from a more recent data cut-off will be available for the presentation.
Keywords : Zanubrutinib, Venetoclax, CLL
Please indicate how this research was funded.:
Please indicate the name of the funding organization. : BeOne Medicines Ltd