Authors
John F. Seymour, MD, Andrew Aw, MD, Vincent Ribrag, MD, PhD, Guillaume Cartron, MD, PhD, Arnon Philip Kater, MD, Ki-Seong Eom, MD, Alan Skarbnik, MD, Alessandra Tedeschi, MD, Malgorzata Wach, MD, Jing-Zhou Hou, MD, Arpad Illes, MD, Batul Suterwala, MD, Anthony J. Corry, PharmD, Ellie John, PhD, Toshifumi Fujimori, PhD, Jennifer R. Brown, MD, PhD.
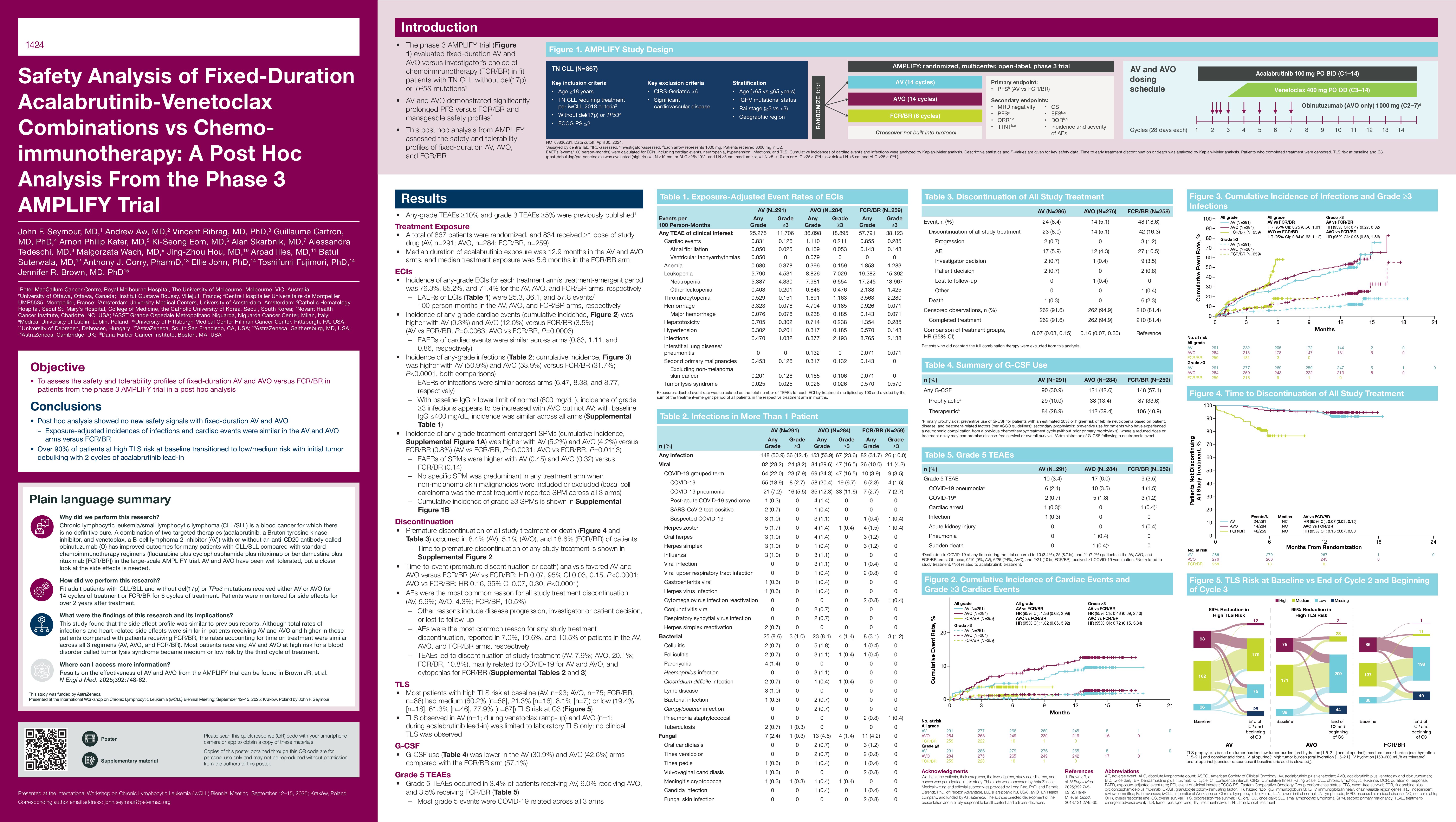
Introduction
The phase 3 AMPLIFY trial evaluated fixed-duration acalabrutinib+venetoclax (AV) or AV+obinutuzumab (AVO) versus fludarabine+cyclophosphamide+rituximab/bendamustine+rituximab (FCR/BR) in fit patients with treatment-naive (TN) chronic lymphocytic leukemia (CLL), where AV and AVO demonstrated prolonged progression-free survival versus FCR/BR and manageable safety profiles (Brown et al. NEJM. 2025). This post hoc analysis from AMPLIFY assesses the safety and tolerability profiles of fixed-duration AV, AVO, and FCR/BR.
Methods
AMPLIFY (ACE-CL-311; NCT03836261) is an ongoing, randomized, open-label, phase 3 trial in patients with TN CLL aged ≥18 years with ECOG performance status ≤2 and without del(17p) or TP53 mutation. Patients were randomized 1:1:1 to receive AV (acalabrutinib, cycles [C] 1–14; venetoclax, C3–14), AVO (AV as described; obinutuzumab, C2−7), or investigator’s choice of chemoimmunotherapy (FCR/BR, C1−6). Exposure-adjusted event rates (EAERs; events/100 person-months) were calculated for treatment-emergent adverse events (AEs) of clinical interest (ECI), including cardiac events, neutropenia, hypertension, infections, and tumor lysis syndrome (TLS). Cumulative incidences of cardiac events and infections were analyzed by Kaplan-Meier analysis (descriptive P-values). TLS risk at baseline and C3 (post-debulking/pre-venetoclax) was evaluated (high risk=lymph node [LN]≥10 cm, or absolute lymphocyte count [ALC]≥25×109/L and LN≥5 cm; medium risk=LN≥5– < 10 cm or ALC ≥25×109/L; low risk=LN < 5 cm and ALC < 25×109/L). Time and cause of early treatment discontinuation or death (combination treatment or any treatment in the regimen) were analyzed; patients who completed treatment were censored.
Results
867 patients were randomized and 834 received ≥1 dose of study drug (AV, n=291; AVO, n=284; FCR/BR, n=259) and were included in this analysis. Median (range) duration of acalabrutinib exposure was 12.9 months (1–18) in AV and 12.9 months (0–18) in AVO; treatment exposure was 5.6 months (1–11) in FCR/BR. Incidence of any-grade ECIs overall was similar with AV (76.3%) versus FCR/BR (71.4%; P=0.229) and higher with AVO (85.2%; P< 0.0001). However, considering exposure duration, EAERs were lower with AV (25.3) and AVO (36.1) versus FCR/BR (57.8). Similarly, cardiac event incidence was higher with AV (9.3%) and AVO (12.0%) versus FCR/BR (3.5%; P≤0.006, both comparisons), whereas EAERs were similar across arms (0.83, 1.11, and 0.86, respectively); any-grade atrial fibrillation, ventricular tachyarrhythmias, and hypertension EAERs were similar across arms (AV, 0.05, 0.05, 0.30; AVO, 0.16, 0.08, 0.32; FCR/BR, 0.14, 0, 0.57, respectively). Any-grade neutropenia EAERs were lower for AV (5.4) and AVO (8.0) versus FCR/BR (17.2). Any-grade infection incidences were higher with AV (50.9%) and AVO (53.9%) versus FCR/BR (31.7%; P< 0.0001, both comparisons), whereas EAERs were similar across arms (6.47, 8.38, and 8.77, respectively). Cumulative infection incidence was similar for AV and AVO versus FCR/BR (HR 0.75, 95% CI 0.56–1.01 and HR 0.84, 95% CI 0.63–1.12, respectively). Infection incidences of any grade (grade ≥3) by pathogen in the AV, AVO, and FCR/BR arms were 8.6% (1.0%), 8.1% (1.4%), and 3.1% (1.2%) (bacterial); 28.2% (8.2%), 29.6% (16.5%), and 10.0% (4.2%) (viral); 2.4% (0.3%), 4.6% (1.4%), and 4.2% (0%) (fungal); and 27.5% (3.8%), 31.3% (6.7%), and 20.5% (4.6%) (unspecified), respectively. Any confirmed/suspected COVID-19 AE was reported in 64 (22.0%) patients in AV, 69 (24.3%) in AVO, and 10 (3.9%) in FCR/BR. Discontinuation of combination treatment or death occurred in 8.4% (AV), 5.1% (AVO), and 18.6% (FCR/BR); time-to-event (discontinuation or death) analysis favored AV and AVO versus FCR/BR (HR 0.07, 95% CI 0.03–0.15; P< 0.0001; HR 0.16, 95% CI 0.07–0.30; P< 0.0001, respectively). AEs were the most common reason for any treatment discontinuation (AV, 7.0%; AVO, 19.6%; FCR/BR, 10.5%), mainly related to COVID-19 for AV and AVO, and cytopenias for FCR/BR. Among patients with high TLS risk at baseline (AV, n=93; AVO, n=75; FCR/BR, n=86), most had medium (60.2%, 21.3%, 8.1%) or low (19.4%, 61.3%, 77.9%) TLS risk at C3. Thus, over 90% at high risk at baseline transitioned to low/medium risk by C3. TLS observed in AV (n=1; during venetoclax ramp-up) and AVO (n=1; during acalabrutinib lead-in) was limited to laboratory TLS only.
Conclusion
This safety analysis from AMPLIFY showed no new safety signals with fixed-duration AV and AVO. Infection incidence was similar to previous reports and cardiac event rates were similar in the AV and AVO arms versus FCR/BR. Over 90% of patients at high TLS risk at baseline transitioned to low/medium risk with initial tumor debulking with 2 cycles of acalabrutinib lead-in.
Keywords : chronic lymphocytic leukemia, safety, fixed duration
Please indicate how this research was funded. : Study funded by AstraZeneca
Please indicate the name of the funding organization.: AstraZeneca