The role of Minimal Residual Disease in chronic lymphocytic leukemia (2MB)
Authors
Ming Liu, Luomengjia Dai, Ziyuan Zhou, Minjie Yu, Shuchao Qi, Yujie Wu, Yi Miao, Yi Xia, Jianyong Li,Huayuan Zhu.
Introduction
Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) are incurable B-cell malignancy with a heterogeneous clinical course especially those with high risk factors. Ibrutinib combined with fludarabine, cyclophosphamide, and rituximab (iFCR) as a time-limited regimen in treatment naïve patients with CLL/SLL demonstrated remarkable efficacy. MRD (Measurable Residual Disease) was considered as a surrogate endpoint of PFS. This study aimed to explore the application of MRD in efficacy assessment, prognostic stratification and discuss the clinical factors influencing the achievement of undetectable MRD (uMRD) under the time-limited therapies based on BTK inhibitors combined with FCR in CLL/SLL.
Methods
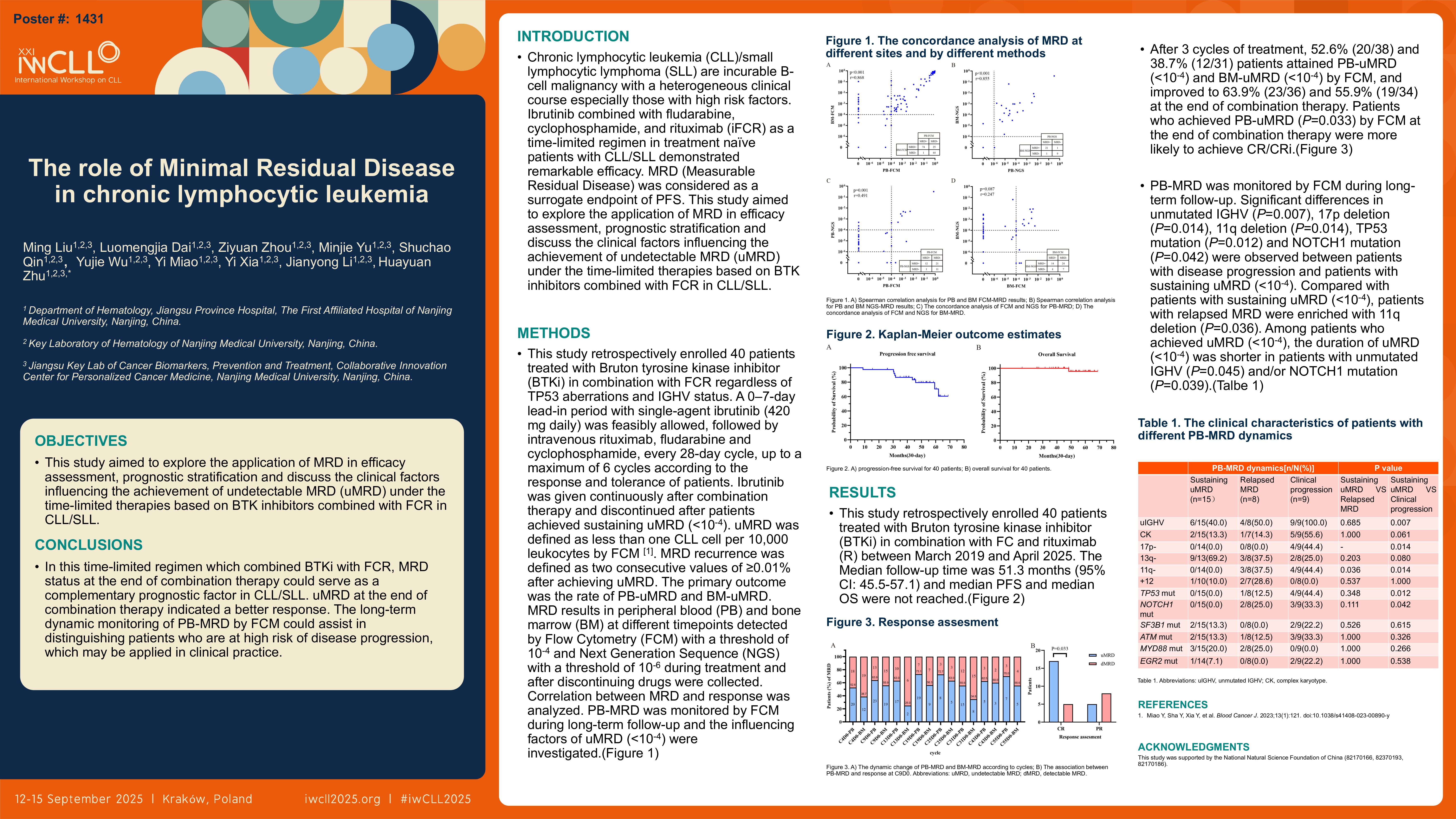
This study retrospectively enrolled 40 patients treated with Bruton tyrosine kinase inhibitor (BTKi) in combination with FCR regardless of TP53 aberrations and IGHV status. A 0–7-day lead-in period with single-agent ibrutinib (420 mg daily) was feasibly allowed, followed by intravenous rituximab, fludarabine and cyclophosphamide, every 28-day cycle, up to a maximum of 6 cycles according to the response and tolerance of patients. Ibrutinib was given continuously after combination therapy and discontinued after patients achieved sustaining uMRD ( < 10-4). uMRD was defined as less than one CLL cell per 10,000 leukocytes by FCM. [Miao Y, Sha Y, Xia Y, et al. Blood Cancer J. 2023;13(1):121. doi:10.1038/s41408-023-00890-y]. MRD recurrence was defined as two consecutive values of ≥0.01% after achieving uMRD. The primary outcome was the rate of PB-uMRD and BM-uMRD. MRD results in peripheral blood (PB) and bone marrow (BM) at different timepoints detected by Flow Cytometry (FCM) with a threshold of 10-4 and Next Generation Sequence (NGS) with a threshold of 10-6 during treatment and after discontinuing drugs were collected. Correlation between MRD and response was analyzed. PB-MRD was monitored by FCM during long-term follow-up and the influencing factors of uMRD ( < 10-4) were investigated.
Results
This study retrospectively enrolled 40 patients treated with Bruton tyrosine kinase inhibitor (BTKi) in combination with FC and rituximab (R) between March 2019 and April 2025. The Median follow-up time was 51.3 months (95% CI: 45.5-57.1) and median PFS and median OS were not reached. After 3 cycles of treatment, 52.6% (20/38) and 38.7% (12/31) patients attained PB-uMRD ( < 10-4) and BM-uMRD ( < 10-4) by FCM, and improved to 63.9% (23/36) and 55.9% (19/34) at the end of combination therapy. Patients who achieved PB-uMRD (P=0.033) by FCM at the end of combination therapy were more likely to achieve CR/CRi. PB-MRD was monitored by FCM during long-term follow-up. Significant differences in unmutated IGHV (P=0.007), 17p deletion (P=0.014), 11q deletion (P=0.014), TP53 mutation (P=0.012) and NOTCH1 mutation (P=0.042) were observed between patients with disease progression and patients with sustaining uMRD ( < 10-4). Compared with patients with sustaining uMRD ( < 10-4), patients with relapsed MRD were enriched with 11q deletion (P=0.036). Among patients who achieved uMRD ( < 10-4), the duration of uMRD ( < 10-4) was shorter in patients with unmutated IGHV (P=0.045) and/or NOTCH1 mutation (P=0.039).
Conclusions
In this time-limited regimen which combined BTKi with FCR, MRD status at the end of combination therapy could serve as a complementary prognostic factor in CLL/SLL. uMRD at the end of combination therapy indicated a better response. The long-term dynamic monitoring of PB-MRD by FCM could assist in distinguishing patients who are at high risk of disease progression, which may be applied in clinical practice.
Keywords : CLL/SLL, MRD, Combination therapy
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: