Authors
Talha Munir, David Cairns, Natasha Greatorex, Rhiannon Lambkin, Sharon Jackson, Annah Muli, Dex Everritt, Colleen Sellwood, Andy Rawstron, Bryony Dawkins, David Allsup, Adrian Bloor, Lelia Duley, Hilary Lindsay.
Design
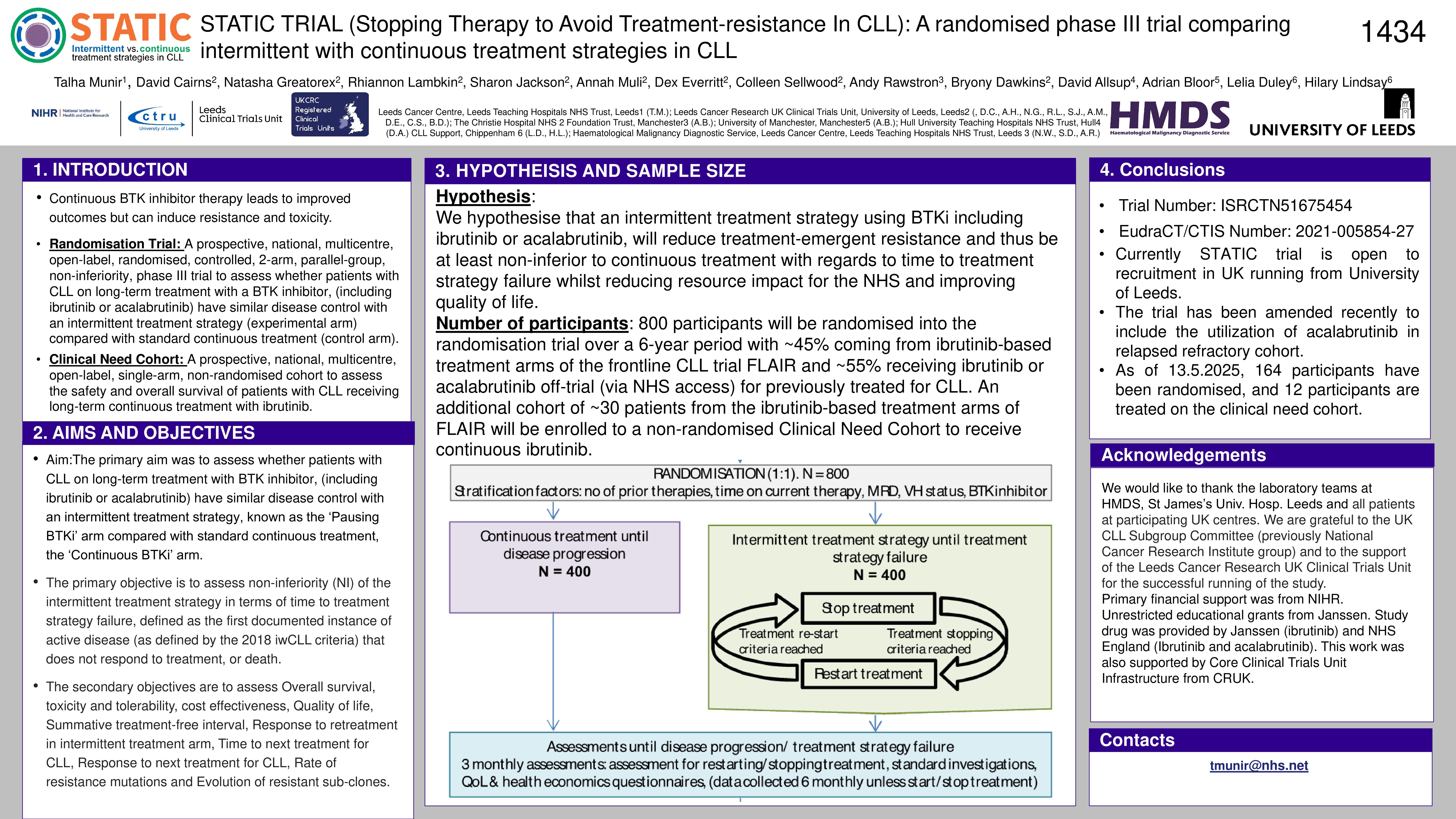
STATIC is designed with multiple pathways, the ‘Randomisation Pathway’ and the ‘Clinical Need Cohort’ – which route a participant enters will be determined by their eligibility.
Randomisation Pathway
A prospective, national, multicentre, open-label, randomised, controlled, 2-arm, parallel-group, non-inferiority, phase III trial to assess whether patients with CLL on long-term treatment with a BTK inhibitor, (including ibrutinib or acalabrutinib) have similar disease control with an intermittent treatment strategy (experimental arm) compared with standard continuous treatment (control arm).
Clinical need cohort
A prospective, national, multicentre, open-label, single-arm, non-randomised cohort to assess the safety and overall survival of patients with CLL receiving long-term continuous treatment with ibrutinib.
Aims and objectives
The primary aim was to assess whether patients with CLL on long-term treatment with BTK inhibitor, (including ibrutinib or acalabrutinib) have similar disease control with an intermittent treatment strategy, known as the ‘Pausing BTKi’ arm compared with standard continuous treatment, the ‘Continuous BTKi’ arm.
The primary objective is to assess non-inferiority (NI) of the intermittent treatment strategy in terms of time to treatment strategy failure, defined as the first documented instance of active disease (as defined by the 2018 iwCLL criteria) that does not respond to treatment, or death.
The secondary objectives are to assess Overall survival, toxicity and tolerability, cost effectiveness, Quality of life, Summative treatment-free interval, Response to retreatment in intermittent treatment arm, Time to next treatment for CLL, Response to next treatment for CLL, Rate of resistance mutations and Evolution of resistant sub-clones.
Hypothesis
We hypothesise that an intermittent treatment strategy using BTKi including ibrutinib or acalabrutinib, will reduce treatment-emergent resistance and thus be at least non-inferior to continuous treatment with regards to time to treatment strategy failure whilst reducing resource impact for the NHS and improving quality of life.
Number of participants
800 participants will be randomised into the randomisation trial over a 6-year period with ~45% being front-line CLL participants receiving treatment with ibrutinib as their first-line and only line of treatment and ~55% being patients receiving ibrutinib or acalabrutinib off-trial (via NHS access) for previously treated for CLL. An additional cohort of ~30 patients from the ibrutinib-based treatment arms of FLAIR and IcICLLe will be enrolled to a non-randomised Clinical Need Cohort to receive continuous ibrutinib.
Current recruitment
Currently STATIC trial is open to recruitment in UK running from University of Leeds. The trial has been amended recently to include the utilization of acalabrutinib in relapsed refractory cohort. As of 29.5.2025, 168 participants have been randomised, and 12 participants are treated on the clinical need cohort.
Keywords : front-line, relapsed/refractory, BTK inhibitor
Please indicate how this research was funded.: Primary financial support is provided by the NIHR Health Technology Assessment Programme and Janssen Pharmaceutical Companies of Johnson & Johnson.
Please indicate the name of the funding organization. : Primary financial support is provided by the NIHR Health Technology Assessment Programme and Janssen Pharmaceutical Companies of Johnson & Johnson.