Authors
Miguel Bastos Boente, María García Álvarez, Cristina Jiménez Sánchez, Alicia Antón Gómez, Ana Balanzategui Echevarría, María Eugenia Alonso Sarasquete, Alejandro Herrera Medina, Rebeca Maldonado Sánchez, María Jesús Vidal Manceñido, Abelardo BárezGarcía, Ana Smucler Simonovich, María Jesús Peñarrubia Ponce, Emilia Pardalde la Mano, José Antonio Queizán Hernández, Francisco Javier Díaz Gálvez, Alberto AlbarránSevero, Carlos Aguilar Franco, Luis García Martín, Ramón García Sanz, Cristina de Ramón Sánchez, Norma Carmen Gutiérrez Gutiérrez, Almudena Navarro Bailón, Miguel Alcoceba Sánchez.
Introduction
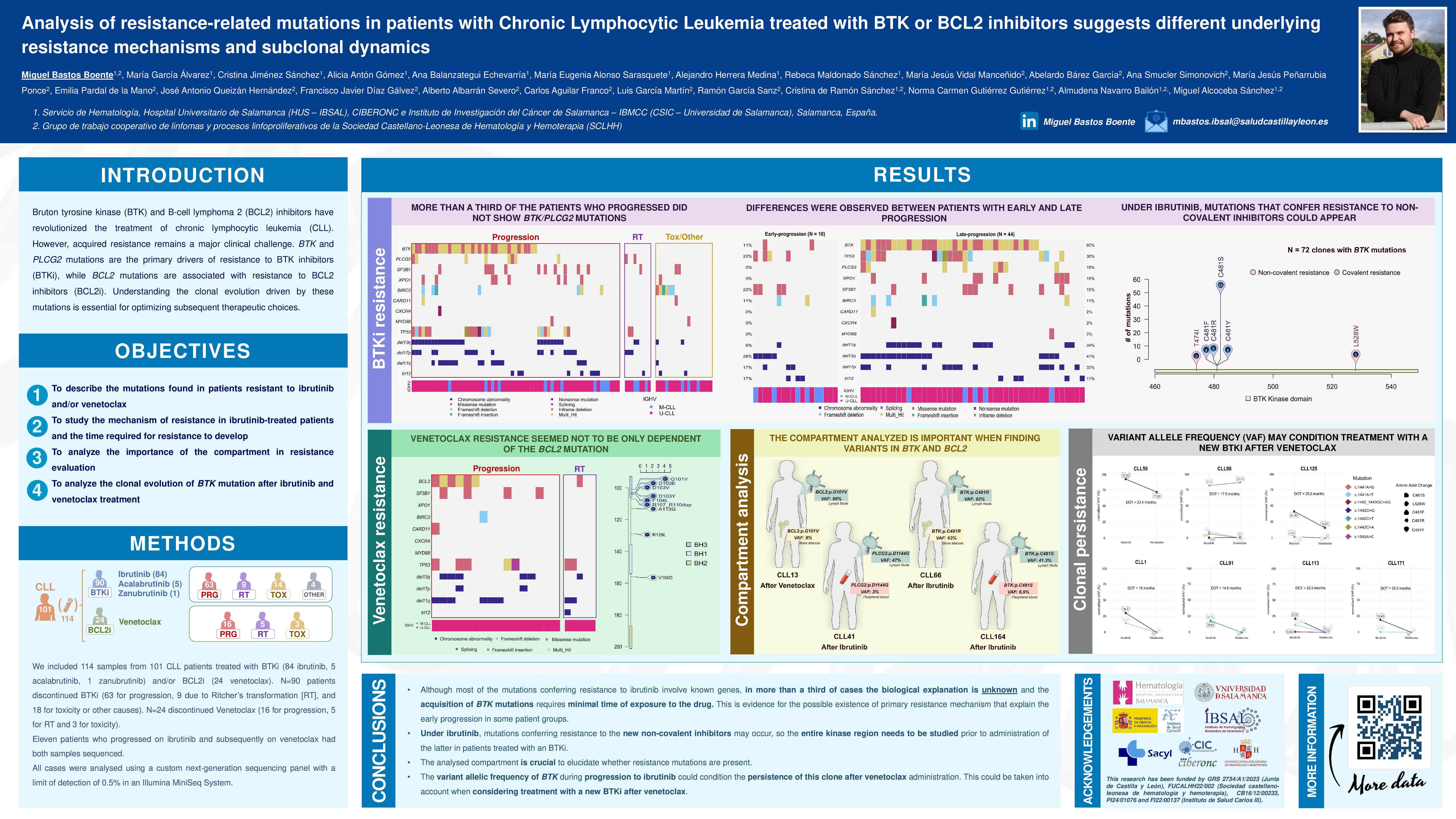
Bruton tyrosine kinase (BTK) and B-cell lymphoma 2 (BCL2) inhibitors have revolutionized the treatment of chronic lymphocytic leukemia (CLL). However, acquired resistance remains a major clinical challenge. BTK and PLCG2 mutations are the primary drivers of resistance to BTK inhibitors (BTKi), while BCL2 mutations are associated with resistance to BCL2 inhibitors (BCL2i). Understanding the clonal evolution driven by these mutations is essential for optimizing subsequent therapeutic choices.
Objectives
To characterize the mutational landscape of CLL patients who discontinued BTKi and/or BCL2i due to progression, transformation, or toxicity. Specific aims included: (i) evaluating the frequency and distribution of BTK and PLCG2 mutations in patients progressing on BTKi; (ii) identifying BCL2 mutations and their impact on venetoclax resistance; (iii) analyzing the relationship between duration of treatment (DOT) and mutation emergence; and (iv) exploring the persistence of mutated clones post-progression and their impact on following therapies.
Methods
We included 114 samples from 101 CLL patients treated with BTKi (84 ibrutinib, 5 acalabrutinib, 1 zanubrutinib) and/or BCL2i (24 venetoclax). A total of 90 patients discontinued BTKi (63 for progression, 9 for Richter’s transformation [RT], and 18 for toxicity/other causes), and 24 discontinued venetoclax (16 for progression, 5 for RT, and 3 for toxicity). Eleven patients who progressed on ibrutinib and subsequently on venetoclax had both samples sequenced. All cases were analyzed using a custom next-generation sequencing (NGS) panel with a limit of detection of 0.5% in an Illumina MiniSeq System.
Results
Among the patients that progressed under BTKi, we found BTK/PLCG2 mutations in 39/63 patients (61.9%). Moreover, BTK/PLCG2 mutations were underrepresented in RT patients in comparison to patients that progressed (22.2% vs. 61.9%, p< 0.05). Mutations in BTK/PLCG2 were totally absent in toxicity cases.
Progression under BTKi displayed a bimodal distribution, distinguishing late progressors (LP, DOT>24 months) from early progressors (EP, DOT < 24 months) (median DOT 57.0 vs. 10.0 months, p< 0.001). LP patients showed a markedly higher frequency of BTK/PLCG2 mutations compared to EP patients (81.8% vs. 11.1%; p< 0.001). Similarly, they were more likely to appear in late-transformed patients with a higher DOT in BTK/PLCG2 mutated cases (median DOT 36.8 vs. 7.2 months, p=0.056).
NGS revealed 72 BTK-mutated clones, predominantly affecting cysteine 481 (n=68; 94.4%), with the C481S mutation as the most frequent (n=55; 76.4%). Additionally, resistance-associated mutations against non-covalent BTKi were identified in 7% of cases (L528W: 4.2%; T474I: 2.8%). In the case of PLCG2-mutated cases, we found 24 clones, whose mutations were mainly within the SH2 domain (41.7%).
Among the 16 patients that progressed after venetoclax, 37.5% (n=6) presented BCL2 mutations. We identified 16 clones, being the most prevalent mutation G101V (n=4; 25.0%). No significant differences were observed in the frequency of mutations between RT and non-RT cases (37.5% vs. 20.0%; p=0.62) or between LP and EP (33.3% vs. 37.5%; p=1.0).
Additionally, we analyzed four patients with mutations in BTK, PLCG2, or BCL2 across two distinct anatomical compartments. Two of these cases had developed Richter’s transformation (RT) after ibrutinib or venetoclax treatment, whereas the others had experienced nodal progression following ibrutinib therapy. Notably, differences in the infiltration of the resistant clone were observed across compartments in all four cases, with the disparity being particularly pronounced in RT, where the resistant clone showed a marked increase in nodal versus non-nodal samples. This finding highlights the importance of studying the compartment with the highest tumor burden, when possible.
For the eleven patients who progressed on BTKi and then on venetoclax, seven of them carried, at least, one BTK mutated clone prior to venetoclax treatment. BTK-mutated clones persisted in three cases (42.9%), with those exhibiting a higher variant allele frequency (normalized VAF>40%) more likely to remain as dominant clones.
Conclusions
Our study highlights the complexity of resistance mechanisms in CLL, particularly with the emergence of different resistance pathways in BTKi-treated patients. Cross-resistance to next-generation non-covalent BTKi may arise under ibrutinib treatment. The tumor burden of BTK-mutated clones prior to venetoclax initiation appears to influence their persistence post-treatment, potentially affecting the efficacy of future therapies. These findings underscore the need for precise molecular monitoring and tailored therapeutic strategies to overcome resistance in CLL.
Keywords : Resistance, relapsed/refractory, sequencing
Please indicate how this research was funded. : The study was funded by Junta de Castilla y León (GRS2734/A1/2023). First author contract was funded by the Instituto de Salud Carlos III (ISCIII) via Instituto de Investigación Biomédica de Salamanca (IBSAL) through a PFIS contract (PI22/000137).
Please indicate the name of the funding organization.: Junta de Castilla y León; Instituto de Salud Carlos III (ISCIII); Gobierno de España