Authors
Zulfa Omer, Alexey Danilov, Francesco Forconi, Nirav Shah, Graham P. Collins, Shuo Ma, Jane Robertson, Alvaro Alencar, Danielle Brander, John C. Byrd, Dima El-Sharkawi, Jeffery Smith, Allison Winter, Michal Kwiatek, Jonathon Cohen, Prioty Islam, Sarah Injac, Talha Munir.
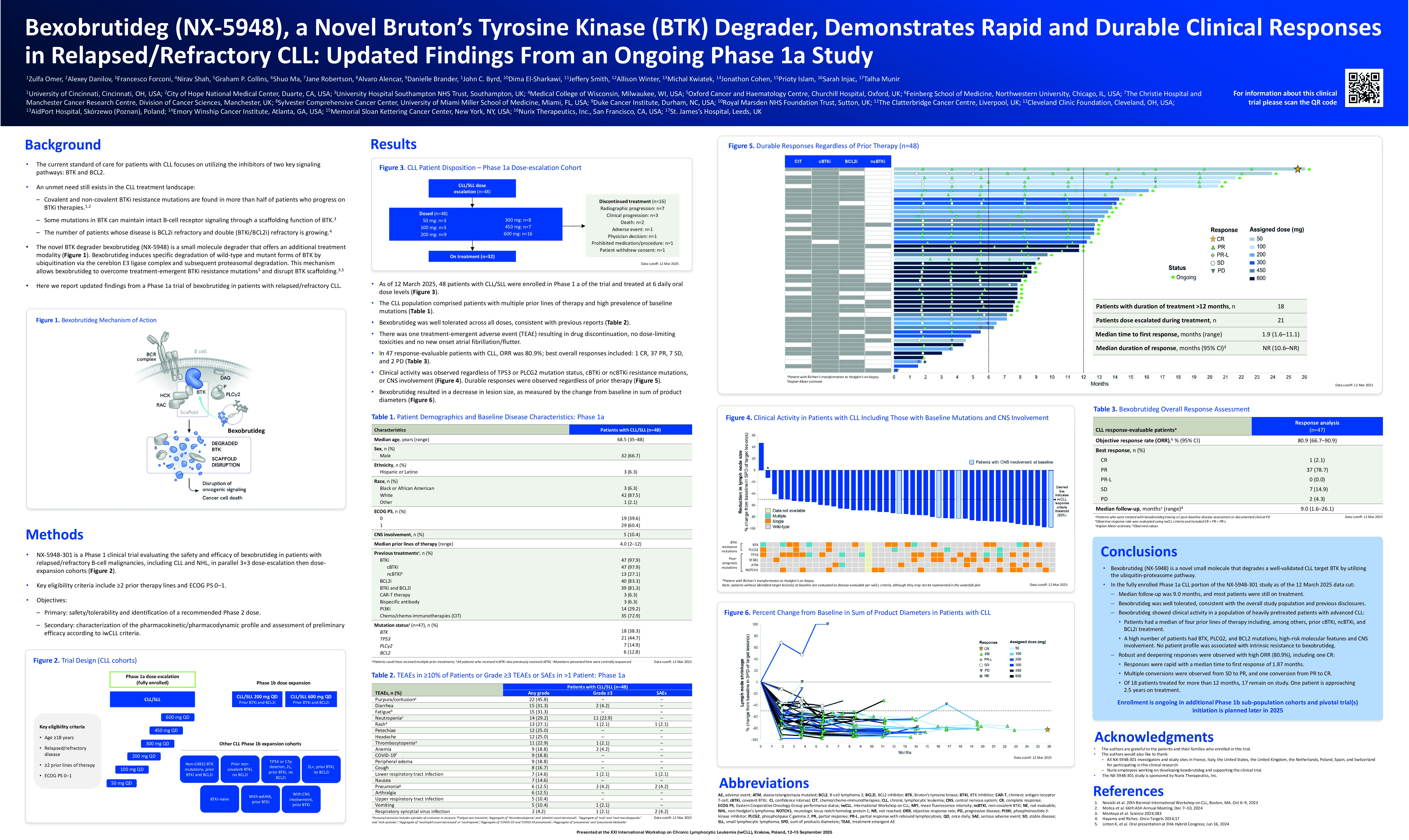
Background
Although BTK inhibition has proven to be a successful treatment modality in CLL, the emergence of BTK inhibitor (BTKi) resistance mutations and identification of kinase-independent signaling via the scaffolding function of BTK underscores the need for alternative approaches to target the totality of BTK protein functions. Bexobrutideg is a novel, orally administered small molecule degrader that induces removal of wild-type and mutant forms of BTK through ubiquitination by the cereblon E3 ligase complex and subsequent proteasomal degradation. We report updated findings from a Phase 1a trial of bexobrutideg in patients with relapsed/refractory (R/R) CLL.
Methods
NX-5948-301 is a Phase 1, first-in-human trial of bexobrutideg in R/R B-cell malignancies, including CLL and NHL/WM, in parallel 3+3 dose-escalation (1a) and dose-expansion (1b) cohorts. Key eligibility criteria include ≥2 prior therapy lines that included a BTKi and ECOG PS 0–1. Primary objectives are evaluation of safety/tolerability and identification of a recommended Phase 2 dose. Key secondary objectives include characterization of the PK/PD profile and assessment of preliminary efficacy according to iwCLL criteria.
Results
As of the 2 January 2025 cutoff date, the Phase 1a cohort was fully enrolled including 48 patients with CLL/SLL who were treated at 6 dose levels p.o. daily: 50 mg (n=3), 100 mg (n=5), 200 mg (n=9), 300 mg (n=8), 450 mg (n=7), 600 mg (n=16). Median age was 68.5 (range 35–88) years; 66.7% were male; there was a median of 4 (range 2–12) prior lines of therapy, including: cBTKi (97.9%), ncBTKi (27.1%), BCL2i (83.3%), BTKi+BCL2i (81.3%), chemo/chemoimmunotherapy (72.9%), PI3Ki (29.2%), and CAR-T (6.3%). In 47 patients with genetic testing available at baseline, mutations identified were: TP53 (44.7%), BTK (38.3%), PLCG2 (14.9%), and BCL2 (12.8%).
Bexobrutideg was well tolerated across all doses in the Phase 1a CLL cohort (n=48), consistent with the overall study safety population. The median duration of treatment was 7.0 (range 0.2–23.8) months. There were no DLTs; 1 patient discontinued due to a TEAE. The most common TEAEs were: purpura/contusion (41.7%, no Gr≥3); fatigue (31.3%, no Gr≥3); neutropenia (29.2%, 22.9% Gr≥3); rash (29.2%, 2.1% Gr≥3, 2.1% SAE), diarrhea (29.2%; 4.2% Gr≥3), and petechiae (25.0%, no Gr≥3). One Grade 5 event (pulmonary embolism, considered unrelated to bexobrutideg) occurred in a patient with a history of atrial fibrillation. No systemic fungal infections or new onset atrial fibrillation were observed.
In 47 response-evaluable patients with CLL from the Phase 1a cohort, the ORR was 80.9% (all PR). Responses were rapid with a median time to first response of 1.9 (range 1.6–11.1) months. Median duration of response has not been reached. Thirteen patients have reached >12 months on study, and 5 patients >18 months. Durable responses were seen regardless of prior treatments, mutations in TP53, PLCG2, BCL2 and BTK (including kinase active and kinase dead), or CNS involvement.
Conclusions
Bexobrutideg was well tolerated in patients with R/R CLL, including those with longer duration of treatment and higher doses. In this fully enrolled Phase 1a cohort, bexobrutideg showed rapid and durable responses independent of prior treatment or high-risk features such as double refractory status and unfavorable genetic profile. Phase 1b dose expansion (200 and 600 mg cohorts) is underway with plans to initiate pivotal trials in 2025.
Keywords : Bexobrutideg, NX-5948, BTK degrader
Please indicate how this research was funded.: Pharmaceutical company
Please indicate the name of the funding organization. : Nurix Therapeutics