Authors
Tomas Arpas, Anna Panovska, Lenka Polcerova, Martin Spacek, Tereza Shokralla, Martin Simkovic, Pavel Vodarek, Jana Mihalyova, Jana Zuchnicka, Daniel Lysak, Lekaa Mohammad, Heidi Mocikova, Tomas Papajik, Zuzana Kubova, Martin Brejcha, Adriana Heindorfer, Lukas Stejskal, Hynek Poul, Denisa Bakesova, Maria Bucikova, Eva Ondrouskova, Jitka Malcikova, Sarka Pavlova, Michael Doubek.
Introduction
Real-world evidence (RWE) analyses of unselected patient populations offer valuable insights into the effectiveness and safety of Bruton tyrosine kinase inhibitors (BTKi) in relapsed/refractory chronic lymphocytic leukemia (R/R CLL), supplementing data from randomized clinical trials.
Methods
We conducted a retrospective analysis using data from the Czech CLL Patients Registry (CLLEAR). Adult R/R CLL patients treated with either ibrutinib or acalabrutinib at one of eleven Czech hematology centers between December 2015 and June 2024 were included. All patients met the International Workshop on CLL (iwCLL) diagnostic criteria and had provided informed consent. The analysis endpoints included overall response rate (ORR), time to next treatment (TTNT), overall survival (OS), and adverse event (AE) incidence. Treatment response was evaluated per iwCLL 2008 criteria. TTNT was defined as the time from BTKi initiation to either subsequent treatment or death. TTNT and OS were estimated using the Kaplan-Meier method. AEs were graded using CTCAE v5.0, with a focus on atrial fibrillation, hypertension, bleeding, and infections. The impact of molecular risk factors (17p deletion and/or TP53 mutation, IGHV mutational status), clinical risk factors (bulky disease; Cumulative International Rating Scale, CIRS > 6), and treatment-related toxicity on TTNT and OS was also evaluated.
Results
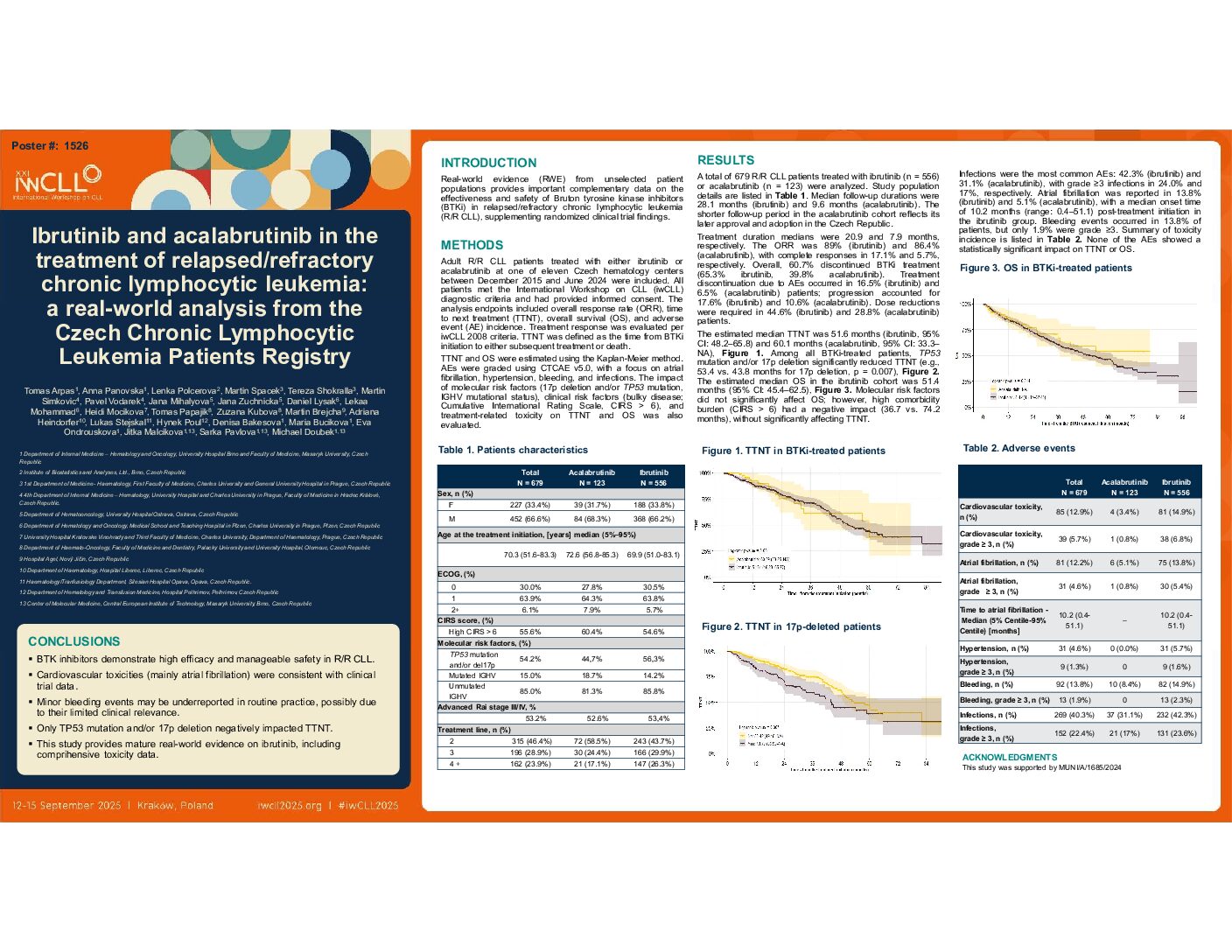
A total of 679 R/R CLL patients treated with ibrutinib (n = 556) or acalabrutinib (n = 123) were analyzed. Median age at BTKi initiation was 69.9 years for ibrutinib and 72.6 years for acalabrutinib; males predominated in both groups (66.2% vs. 68.3%). High comorbidity burden (CIRS > 6) was observed in over half the cohort (54.6% vs. 60.4%), and the majority had advanced Rai stage III/IV disease (53.4% vs. 52.6%). The median number of prior treatment lines was 2 in both cohorts. Adverse molecular risk features were common: unmutated IGHV was present in 85.8% (ibrutinib) and 81.3% (acalabrutinib), while 17p deletion and/or TP53 mutations were seen in 56.3% and 44.7%, respectively. Isolated TP53 mutation was detected only in 11.7% (ibrutinib) and 6.5% (acalabrutinib) patients.
Median follow-up durations were 28.1 months (ibrutinib) and 9.6 months (acalabrutinib). Treatment duration medians were 20.9 and 7.9 months, respectively. The ORR was 89% (ibrutinib) and 86.4% (acalabrutinib), with complete responses in 17.1% and 5.7%, respectively. Overall, 60.7% discontinued BTKi treatment (65.3% ibrutinib, 39.8% acalabrutinib). Treatment discontinuation due to AEs occurred in 16.5% (ibrutinib) and 6.5% (acalabrutinib) patients; progression accounted for 17.6% (ibrutinib) and 10.6% (acalabrutinib). Dose reductions were needed in 44.6% (ibrutinib) and 28.8% (acalabrutinib) patients.
The estimated median TTNT was 51.6 months (ibrutinib, 95% CI: 48.2–65.8) and 60.1 months (acalabrutinib, 95% CI: 33.3–NA). Among all BTKi-treated patients, TP53 mutation and/or 17p deletion significantly reduced TTNT (e.g., 53.4 vs. 43.8 months for 17p deletion, p = 0.007). The estimated median OS in the ibrutinib cohort was 51.4 months (95% CI: 45.4–62.5). Molecular risk factors did not significantly affect OS; however, high comorbidity burden (CIRS > 6) had a negative impact (36.7 vs. 74.2 months), without significantly affecting TTNT.
Infections were the most common AEs: 42.3% (ibrutinib) and 31.1% (acalabrutinib), with grade ≥3 infections in 24.0% and 17%, respectively. Atrial fibrillation was reported in 13.8% (ibrutinib) and 5.1% (acalabrutinib), with a median onset time of 10.2 months (range: 0.4–51.1) post-treatment initiation in the ibrutinib group. Bleeding events occurred in 13.8% of patients, but only 1.9% were grade ≥3. None of the AEs showed a statistically significant impact on TTNT or OS.
Conclusion
Our real-world data confirm the clinical efficacy and manageable safety profile of BTKi in R/R CLL. The incidence and spectrum of cardiovascular toxicities, particularly atrial fibrillation, were consistent with findings from randomized clinical trials. Minor bleeding events appear underreported, likely due to limited clinical impact or under recognition by clinicians. The shorter follow-up period in the acalabrutinib cohort reflects its later approval and adoption in the Czech Republic, which limits longitudinal comparisons.
Supported by MUNI/A/1685/2024
Keywords : relapsed/refractory, ibrutinib, acalabrutinib
Please indicate how this research was funded. : Funded by grant MUNI/A/1685/2024
Please indicate the name of the funding organization.: Masaryk University in Brno, Czech Republic