Authors
YSEBAERT L, TCHERNONOG E, BOMMIER C, FITOUSSI O, TEXIER N, COINT-BAVAROT M, SANTAGOSTINO A, SAINT-GERARD N, DUPUIS S, KARIYAWASAM T, OLIVIER G, ALBIN N, DELRIEU L.
Introduction
Physical activity (PA) has proven benefits on health-related quality of life (HRQoL), fatigue, and psychological wellbeing in individuals with chronic diseases and solid tumors (Delrieu, 2020; Cheville, 2013). However, evidence in heme cancers, including chronic lymphocytic leukemia (CLL), remains scarce due to limited sample sizes (Knips, 2019). In CLL, only one pilot study combining high-intensity interval and resistance training in 15 patients reported a clinically meaningful HRQoL improvement (Artese, 2022).
The World Health Organization recommends that adults engage in at least 150 to 300 minutes of moderate-intensity PA, or 75 to 150 minutes of vigorous-intensity PA, or an equivalent combination of both throughout the week, to achieve substantial health benefits. However, these guidelines were based on questionnaires and did not include goals for step counts. Recent studies using activity trackers suggest that even lower doses of PA are associated with improved HRQoL (Lee IM, 2025).
The primary objective of the QOLIBRI study is to assess the impact of an individualized physical activity intervention (IPAI), supported by an activity tracker (connected watch) on HRQoL in patients with CLL undergoing treatment with Ibrutinib (I). Indeed, it is essential to preserve the quality of life for patients due to the chronic nature of this disease. The aim of this interim analysis is to evaluate the feasibility of the intervention, focusing on acceptability, adherence, compliance, and participant retention (ibrutinib until PD or ibrutinib + venetoclax [I+V] fixed duration). We report here on the feasibility phase (N=29) of the trial.
Methods
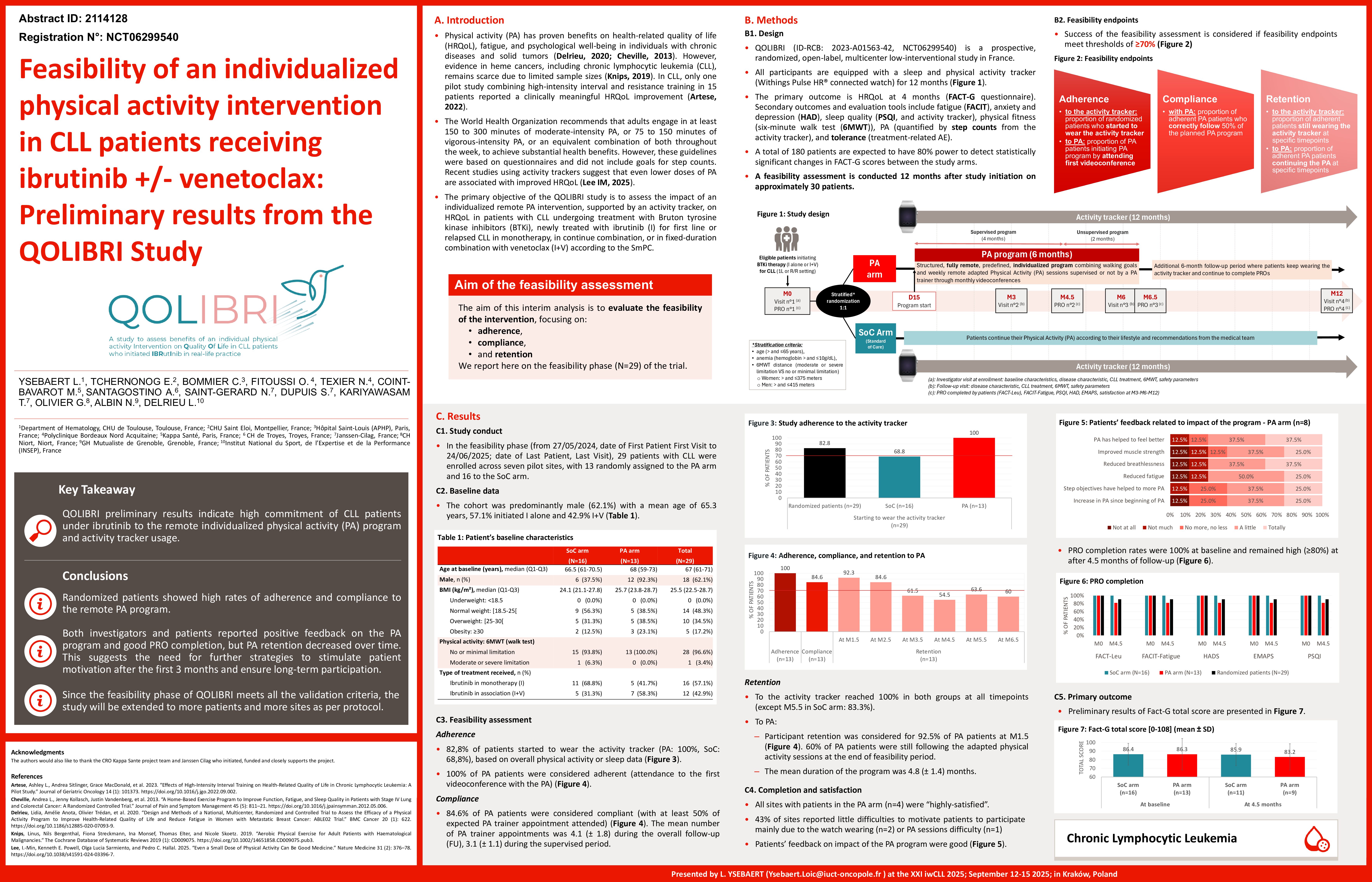
QOLIBRI (ID-RCB: 2023-A01563-42, NCT06299540) is a prospective, randomized, open-label, multicenter low-interventional study in France. Eligible patients initiating BTKi therapy (I alone or I+V) for CLL (1L or R/R setting) are randomized 1:1 to an IPAI or standard of care (SoC) arm. All participants are equipped with an activity tracker for 12 months.
The IPAI group follows a 6-month structured, remote, predefined, individualized program combining walking goals and weekly remote APA sessions supervised by an APA trainer through monthly videoconferences. The intervention is structured into two phases: a four-month supervised period led by the trainer, followed by a two-month unsupervised period designed to promote patient autonomy. Following the 6-month IPAI program, the patients undergo an additional 6-month follow-up period where they keep wearing the activity tracker and continue to complete PROs. In the SoC arm, the patients continue their PA according to their lifestyle and recommendations from the medical team. The primary endpoint is HRQoL at 4.5 months (FACT-G questionnaire). Secondary outcomes and evaluation tools include fatigue (FACIT), anxiety and depression (HAD), sleep quality (PSQI, and activity tracker), physical fitness (six-minute walk test [6MWT]), PA (quantified by step counts from the activity tracker), and tolerance (treatment-related AE). A total of 180 patients are expected to have 80% power to detect statistically significant changes in FACT-G scores between the study arms. A feasibility assessment is conducted 12 months after study initiation on approximately 30 patients to evaluate acceptability (percentage of patients consenting to participate), adherence (percentage of patients from IPAI arm who were actually initiating the IPAI program), compliance (percentage of adherent patients who correctly follow the planned IPAI program), and retention (percentage continuing the IPAI and connected watch use across the different study timepoints).
Results
In the feasibility phase, 29 patients with CLL were enrolled across seven sites, with 13 randomly assigned to the IPAI arm and 16 to the SoC arm. The cohort was predominantly male (62.1%) with a mean age of 65.3 y (range 49-77y), 57,.1% initiated I alone and 42.9% I+V. All patients in the IPAI arm (100%) started the intervention and completed their initial session with the APA trainer. Additionally, 100% of IPAI patients and 93.8% of SoC patients (15 out of 16) began wearing the activity tracker. The complete feasibility assessment is ongoing, and study expansion to all sites will be considered if adherence, compliance, and retention rates exceed 70% during this phase.
Discussion
These preliminary results indicate high adherence to both the IPAI program and activity tracker usage. Complete feasibility results and preliminary efficacy data will be presented during the congress.
Keywords : Chronic Lymphocytic Leukemia; Adapted physical activity; ibrutinib
Please indicate how this research was funded.:
Please indicate the name of the funding organization. :