Authors
Truman Koh, BS; Ashwin Sunderraj, MD; Rudy Mrad, MD; Farrukh T. Awan, MD, MS, MBA
Background
Patients with hematologic malignancies are at significantly higher risk for severe COVID-19 due to disease-related and treatment-induced immunosuppression. Despite widespread vaccine availability, many patients fail to mount effective immune responses. On March 22, 2024, the FDA issued Emergency Use Authorization for pemivibart (Pemgarda™), a long-acting monoclonal antibody for pre-exposure prophylaxis in individuals with moderate-to-severe immunocompromise. While initial approval was based on laboratory and pharmacokinetic data, real-world evidence on Pemivibart’s safety and effectiveness in high-risk populations remains limited. This study evaluates adverse reactions and breakthrough infections following Pemivibart use in immunocompromised patients with hematologic malignancies.
Methods
We analyzed 112 adult patients with lymphoid malignancies who received Pemivibart between March 2024 and May 2025. Clinical data included age, sex, vaccine history, adverse reactions, and incidence of COVID-19 infection after Pemivibart. COVID-19 infection was confirmed through antigen or PCR testing. Descriptive statistics summarized the cohort.
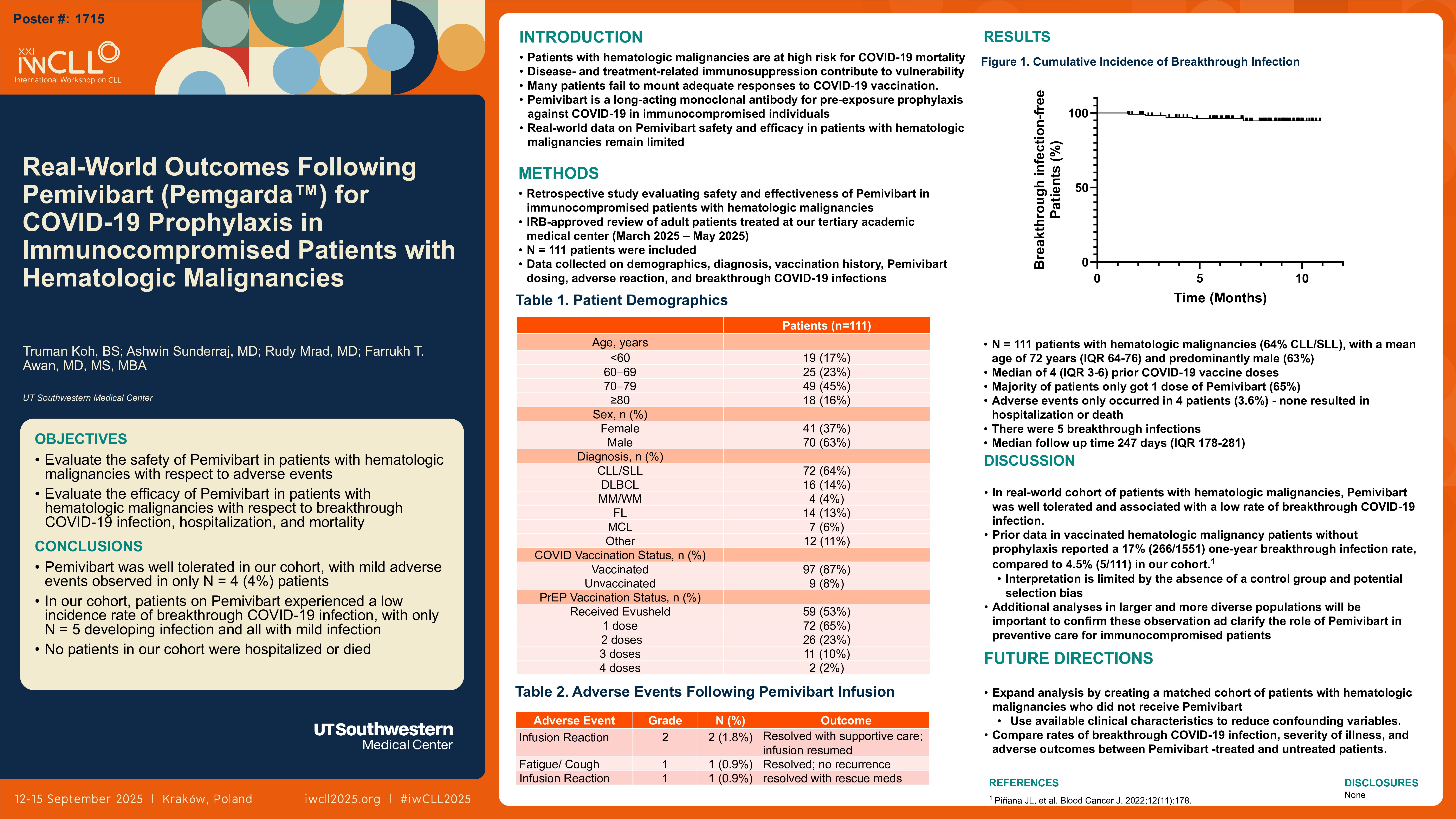
Results
All patients had lymphoid malignancies (CLL, n=69 (62% of the cohort)) at various disease and treatment course points. The mean age was 69.6 years; 48.2% were female. The average number of prior COVID-19 vaccine doses was four, and 34 patients (30.4%) received a second Pemivibart dose. Adverse reactions occurred in 6.3% (7/112), including grade 3 anaphylaxis in one (0.9%) patient that resolved with supportive care, and grade 2 infusion-related reactions in two (1.8%) patients, all of which responded well to supportive care. Three patients (2.7%) developed COVID-19 after Pemivibart administration. Of these, two required hospitalizations: one had no history of vaccination or prior pre-exposure prophylaxis; the other had received two vaccine doses without prior pre-exposure prophylaxis. The third patient, who had three vaccine doses and prior pre-exposure prophylaxis, experienced mild symptoms and recovered with supportive care. No COVID-19-related deaths were reported.
Conclusion
Pemivibart was well-tolerated in immunocompromised patients with lymphoid malignancies, with a low incidence of adverse reactions and breakthrough infections. Hospitalizations occurred only in those with minimal prior immunologic protection, highlighting the continued importance of layered COVID-19 prevention strategies. These real-world findings support using Pemivibart as an adjunct to vaccination in high-risk populations and underscore the need for pre-exposure prophylaxis, especially in patients with a compromised ability to generate adequate vaccine-mediated immunity. Detailed data will be provided at the conference.
Keywords : Pemivibart, COVID-19, lymphoid malignancies, pre-exposure prophylaxis, immunocompromised.
Please indicate how this research was funded. : Not funded
Please indicate the name of the funding organization.: