Authors
Georgios Pongas, Matthew Mei, Lu Chen, Geoffrey Shouse, Rachel Bellsmith, Ivana Borja, Steven Rosen, Tanya Siddiqi, Alexey Danilov.
Background
Chronic lymphocytic leukemia (CLL) is the most common type of adult leukemia in the Western countries and is characterized by the clonal expansion of monoclonal CD5+ and CD19+ B lymphocytes. Despite the advances of the clinical outcomes with the Bruton tyrosine kinase inhibitors (BTKi) and the BCL2 inhibitors (BCL2i), relapses and acquisition of resistance remain a clinical challenge. Therefore, novel therapies in the front-line setting are urgently needed to prolong the survival of the CLL patients and delay the development of progression. CD19 is a B-cell surface antigen expressed in CLL cells which makes it an attractive target for drug development. Tafasitamab is a humanized, FC-enhanced anti-CD19 monoclonal antibody, which has demonstrated favorable response rates and toxicity profile when combined with venetoclax or idelalisib in relapsed and refractory CLL (R/R CLL) (Staber PB et al, ASH 2019). We hypothesized that a time-limited doublet combination of tafasitamab with Zanubrutinib (TaZa) could achieve high efficacy with good tolerability. Herein, we report for first time, the safety and initial preliminary results of TaZa in previously untreated CLL/SLL.
Methods
This is an ongoing multi-center, phase II investigator-initiated trial with safety lead-in of TaZa in treatment-naïve CLL patients (NCT05718869). Eligibility: patients with CLL requiring treatment per iwCLL criteria with ECOG ≤2, creatinine clearance ≥30 ml/min, absolute neutrophil count ≥1000/mm3 and platelet count ≥75,000/mm3. The primary endpoint is to evaluate the safety/tolerability of TaZa in the safety lead-in (6-12 patients) and to assess the complete response in the phase II according to iwCLL 2018 criteria (Hallek M et al, Blood 2018). Patients receive tafasitamab – 12 mg/kg on Cycle 1 Day 1 (C1D1) and C1D4, then weekly in C1-3, every other week in C4-6, and monthly during C7-24. Zanu 160 mg (DL 1) or 80 mg (DL -1) is given orally twice daily. Each cycle is 28 days. All patients continue for at least 12 cycles in the absence of toxicities. Patients who achieve undetectable minimal residual disease (uMRD) status (by clonoSEQ) in the peripheral blood and bone marrow after 12 or 24 cycles of combination therapy will stop both agents. Patients who remain with detectable MRD after 24 cycles may continue treatment with single-agent Zanu for up to a total of 5 years. The study follows Simon’s minimax two-stage design with a total sample size of 25 patients based on a projected CR rate ≥ 30% vs 10% (H0), type I error alpha 9.5% and a power 90%.
Results
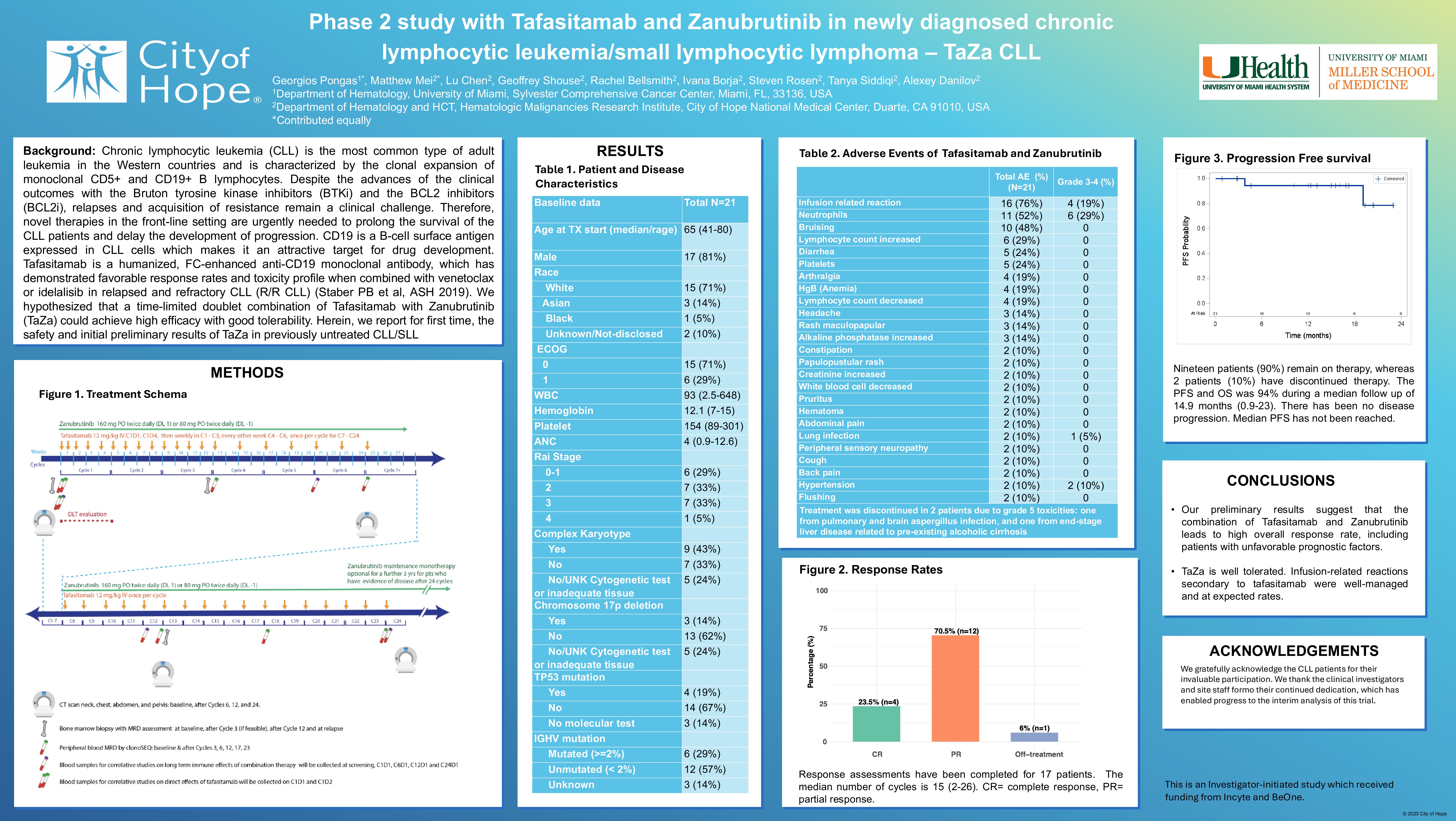
The date for the data cut of this interim analysis was 5/6/2025. Twenty-one patients were enrolled and all were evaluable for safety, with a median follow-up of 14.9 months (range 0.9-23), while 17 patients were evaluable for response. Median age was 65 years (range 41-80); 81% were male; Rai stage 0-1 (29%), 2 (33%) and 3-4 (38%). Baseline prognostic characteristics: unmutated IGVH in 12 pts (57%), TP53 aberrancy in 5 pts (24%) and complex karyotype in 9 pts (43%). The overall response rate was 94% with a CR rate of 24%. The 18-month PFS was 94% (95% CI, 67%-99%). The most frequent any grade AEs have been infusion related reaction (76%), neutropenia (52%) and bruising (48%). The most frequent G3-4 AEs have been neutropenia (29%), infusion related reaction (19%) and hypertension (10%). One patient developed atrial fibrillation.
Treatment was discontinued in 2 patients as a result of grade 5 toxicities: infection (pulmonary and brain aspergillus) and end-stage liver disease (due to pre-existing alcoholic liver cirrhosis).
Conclusions
Our preliminary results suggest that the combination of tafasitamab and Zanubrutinib leads to high overall response rate, including patients with unfavorable prognostic factors. TaZa is well tolerated with no unexpected toxicity. Updated response data with additional patients and correlative MRD studies will be presented in the meeting.
Keywords : CLL, zanubrutinib, tafasitamab
Please indicate how this research was funded.: This study is funded by Incyte
Please indicate the name of the funding organization. : Incyte