Authors
Can Zhang, Othman Al-Sawaf, Mohammad S. Esfahani, Chih Long Liu, Sandra Robrecht, Eugen Tausch, Anke Schilhabel, Matthias Ritgen, Christof Schneider, Martin Peifer, Arnon P Kater, John F Seymour, Brenda Chyla, Yanwen Jiang, Barbara Eichhorst, Stephan Stilgenbauer, Michael Hallek, Ash A. Alizadeh, David M. Kurtz, Kirsten Fischer.
Introduction
Measurable residual disease (MRD) status after limited-duration treatment for patients (pts) with CLL is a strong prognostic factor for survival times, but most prognostic indices such as CLL-IPI rely solely on pre-treatment features. To incorporate dynamic MRD data in prognostic models across diverse cancer types including CLL, the continuous individualized risk index was previously proposed (CIRI, Kurtz et al. 2019). CIRI dynamically determines outcome probabilities for individual pts by integrating diverse factors over time, including treatment modality and serial MRD measurements on and post-treatment. Since developed in the context of chemoimmunotherapy we here propose a refined version of CIRI, CIRI2-CLL, in the context of fixed-duration targeted therapy, which includes MRD status on-treatment (interim), at end-of-treatment (EoT) and in addition at 12-month post-EoT (FU12).
Methods
We inferred model parameters from patient level data of the CLL8/10/11 (FC [±rituximab (R)], BR, Clb [±R/Obi], n=614) and MURANO (venetoclax (Ven)-R vs BR, n=299) trials. For previously established factors, including CLL-IPI (age, IGHV, TP53del/mut, Binet/Rai and ß2M), therapy effect, and MRD status (interim and EoT), we used the updated development set from CLL8/10/11. For the therapeutic effect of Ven and MRD status at FU12, we used the MURANO trial data. To capture the nonuniform change in PFS following therapy coinciding with end of fixed-duration therapy, we utilized piecewise proportional hazard modelling with a single change-point at 18 months in a modified Bayesian model. We then applied the refined model CIRI2-CLL to an independent validation set from the CLL14 study (Ven-Obi vs Clb-Obi, n=381) to predict progression-free survival (PFS) and overall survival (OS). Model calibration, stratification and performance were assessed and compared to individual indices.
Results
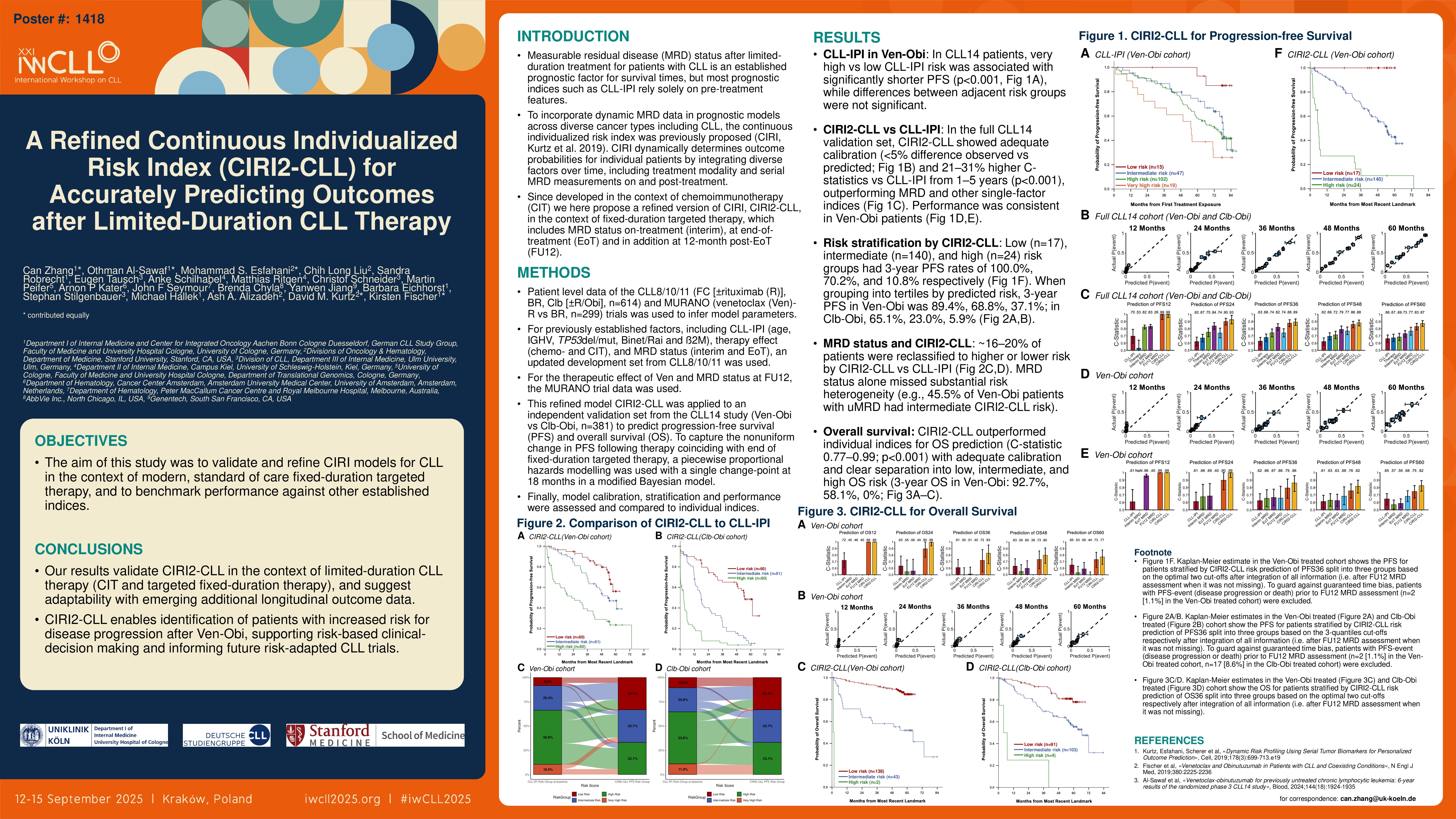
We first applied CLL-IPI (previously established for chemoimmunotherapy) to CLL14 pts treated with Ven-Obi, and observed significantly shorter PFS (p < 0.001) in comparing pts with very high vs low risk. Outcomes of pts with very high or high (p=0.11), high or intermediate CLL-IPI (p=0.41) were similar.
We tested whether CIRI2-CLL improves upon CLL-IPI by comparing their prognostic values in the full CLL14 validation set. CIRI2-CLL demonstrated good calibration with < 5% difference between observed and predicted event probabilities. The performance was significantly improved compared to CLL-IPI as shown by 21-31% improvements in the C-statistic from 1-5 years, including superior prediction to single-factor indices, such as MRD. Performance was maintained when limiting to the Ven-Obi treated pts only. When stratifying pts by CIRI2-CLL into low (17pts), intermediate (140 pts) and high-risk (24 pts) groups on the basis of optimal separation of PFS, the corresponding 3-year PFS rates from most recent landmark were 100%, 70% and 11%.
Furthermore, CIRI2-CLL allows for patient stratification according to 3-quantiles (3-year PFS rate from most recent landmark 89.4%, 68.8% and 37.1% respectively in Ven-Obi treated pts, 3-year PFS rate from most recent landmark 65.1%, 23.0% and 5.9% respectively in Clb-Obi treated pts). Nine (19.6%) and 7 (15.6%) pts with intermediate CLL-IPI risk had high CIRI2-CLL risk in the Ven-Obi cohort and Clb-Obi cohort respectively. Nineteen (18.8%) pts in Ven-Obi and 17 (17.5%) pts in Clb-Obi with high CLL-IPI risk had low CIRI2-CLL risk. In the Ven-Obi cohort, 50 (45.5%) of the pts with undetectable ( < 10-4) MRD at FU12 had intermediate CIRI2-CLL risk. In the Clb-Obi cohort, 30 (33.7%) of the pts with detectable MRD at FU12 had low CIRI2-CLL risk.
For OS, stratification of risk by CIRI2-CLL significantly improved compared to any individual index as seen by a C-statistic between 0.77 and 0.99 at all timepoints, with good calibration (≤ 5% difference from 1-5 years between observed and predicted event probabilities in Ven-Obi treated pts) and clear risk stratification into low, intermediate and high CIRI2-CLL OS risk (3-year OS rate from most recent landmark 92.7%, 58.1% and 0% respectively in Ven-Obi treated pts).
Conclusions
Our results validate CIRI2-CLL in the context of limited-duration CLL therapy, and suggest adaptability with emerging additional longitudinal outcome data. Upon risk stratification, pts with increased risk for disease progression after Ven-Obi can be reliably identified, providing benefits for clinical routine care and important implications for future risk-adapted CLL trials.
Keywords : leukemia, dynamic prognostic index including measurable residual disease, fixed-duration targeted therapy
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: