Authors
Luca Laurenti, Feliciana Guglielmi, Antonio Mosca, Candida Vitale, Maria Chiara Montalbano, Gianmarco Favrin, Isacco Ferrarini, Andrea Galitzia, Raffaella Pasquale, Massimo Moratti, Gioacchino Catania, Roberta Murru, Diana Giannarelli, Enrica Antonia Martino, Riccardo Moia, Antonella Zucchetto, ErikaTissino, Francesco Autore, Annamaria Tomasso, Luca Stirparo, Tommaso Quaranta, Pierluigi Abate, Valter Gattei, Gianluca Gaidano, Massimo Gentile, Mauro Krampera, Giuliana Farina, Varettoni Marzia, Marta Coscia, Idanna Innocenti.
Background
Covalent Bruton tyrosine kinase inhibitors (cBTKi) are a class of drugs that have revolutionized Chronic Lymphocytic Leukemia (CLL) treatment. They target Bruton tyrosine kinase (BTK), an enzyme stimulated by B cell receptor (BCR) activation in B lymphocytes, able to trigger pathways involved in cell surviving, proliferation and migration. BTK inhibition in neoplastic lymphocytes results in their demarginalization from lymph nodes to the peripheral blood. This phenomenon of cell redistribution was widely studied until to define a standard kinetics of lymphocytosis during therapy with cBTKi: an initial further increase of the pre-existing lymphocytosis occurs during the first month of therapy, followed by a gradual reduction over time, sometimes until to the normalization of the absolute lymphocyte count (ALC).
Methods
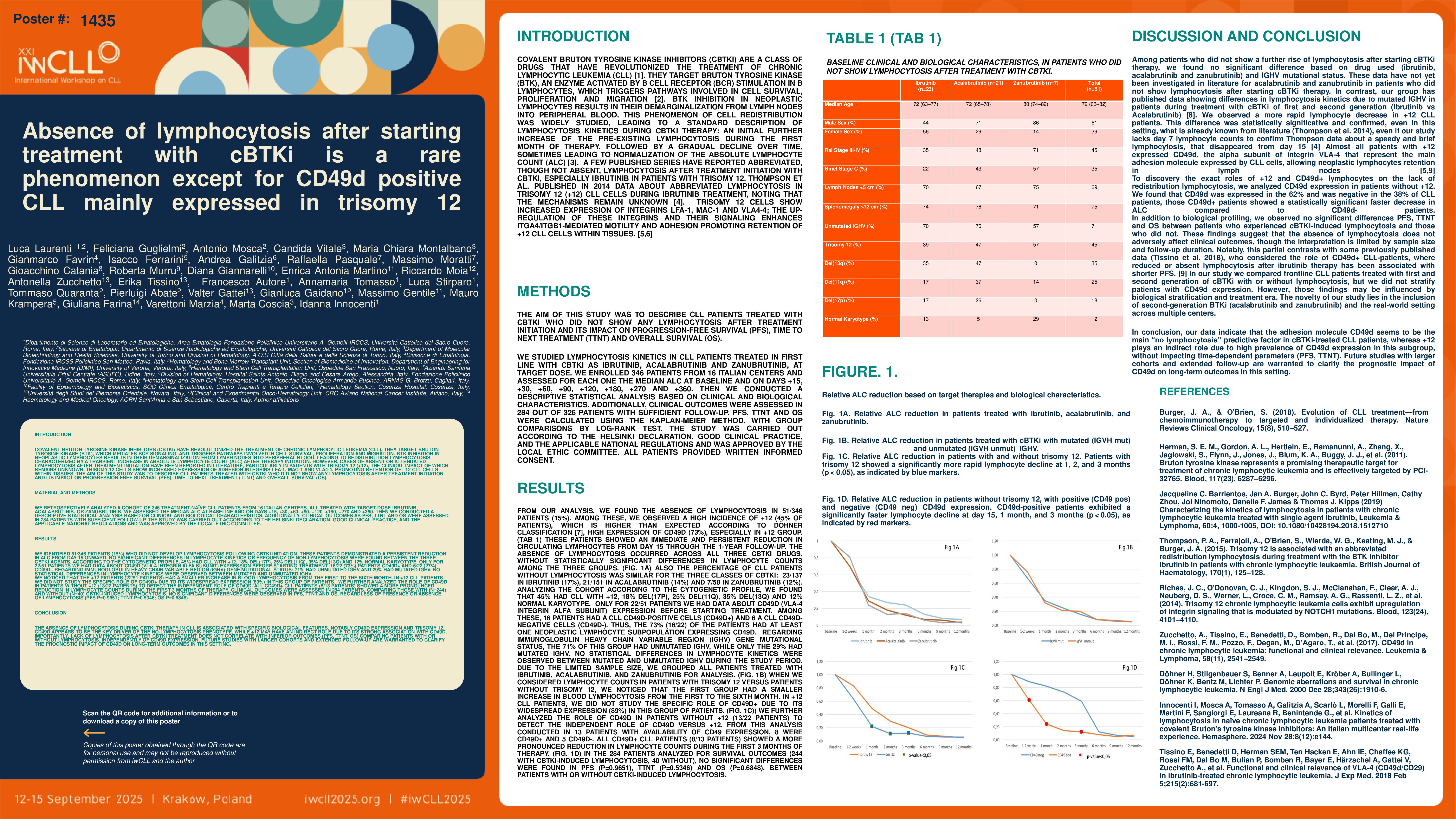
We studied the kinetics of lymphocytosis in patients with CLL treated in I line with Ibrutinib, Acalabrutinib and Zanubrutinib. We enrolled 346 patients from 16 Italian centers, evaluating for each one the median ALC at baseline and at well-defined time-points. Then we carried out a descriptive statistics study.
Results
Analyzing our data, we found an irregular behavior in 51/346 patients: the 15% of patients didn’t show an increase of baseline ALC. Since the beginning they underwent an immediate reduction of circulating lymphocytes. Considering the biological features, the 70.6% of this group of patients was affected by an IGHV unmutated CLL, while only the 27.4% had a IGHV mutated disease. Instead, analyzing the cohort according to the cytogenetic profile, we found that the 44.9% had a CLL with trisomy 12, the 18.4% had a del17p, the 24.5% a del11q, the 34.7% a del13q, the 12.2% a normal karyotype. Only for 24/51 patients we had data about CD49d (VLA-4 integrin alfa subunit) expression before starting treatment. Among these, 15 patients had a CLL CD49d+, 4 a disease CD49d- bimodal and 5 a CLL CD49d-. So, the 79% (19/24) patients had at least a neoplastic lymphocytes’ subpopulation expressing CD49d.
Discussion
Among patients who didn’t show a further rise of lymphocytosis after starting therapy with cBTKi, we didn’t find any significative difference according to drug employed (Ibrutinib, Acalabrutinib or Zanubrutinib) and IGHV mutational status. However, we observed a more rapid lymphocytosis decrease in trisomy 12 CLL patients. This data was statistically significative on days 15-30-60 and confirmed, even in this setting, what is already known from literature (Thompson et al. 2014). All patients (100%) with trisomy 12 showed a complete or partial CD49d expression. Considering the other patients (not trisomy 12), CD49d was expressed in the 65% and was negative in the 35%, and those patients with a CD49d+/CD49d- bim CLL showed a faster decrease in ALC, statistically significative on days 15-30-90, than those ones with a CD49d- CLL. In conclusion, our data suggest that the adhesion molecule CD49d seems to be the main “no lymphocytosis” predictive factor in patients on treatment with cBTKi.
Keywords : Chronic Lymphocytic Leukemia
covalent BTKi
lymphocytosis
Please indicate how this research was funded. : Not funded
Please indicate the name of the funding organization.: Not funded