Authors
Ken Zou, BA; Truman Koh BS; Rudy Mrad, MD; Heather R. Wolfe, MD; Farrukh T. Awan, MD, MS, MBA
Background
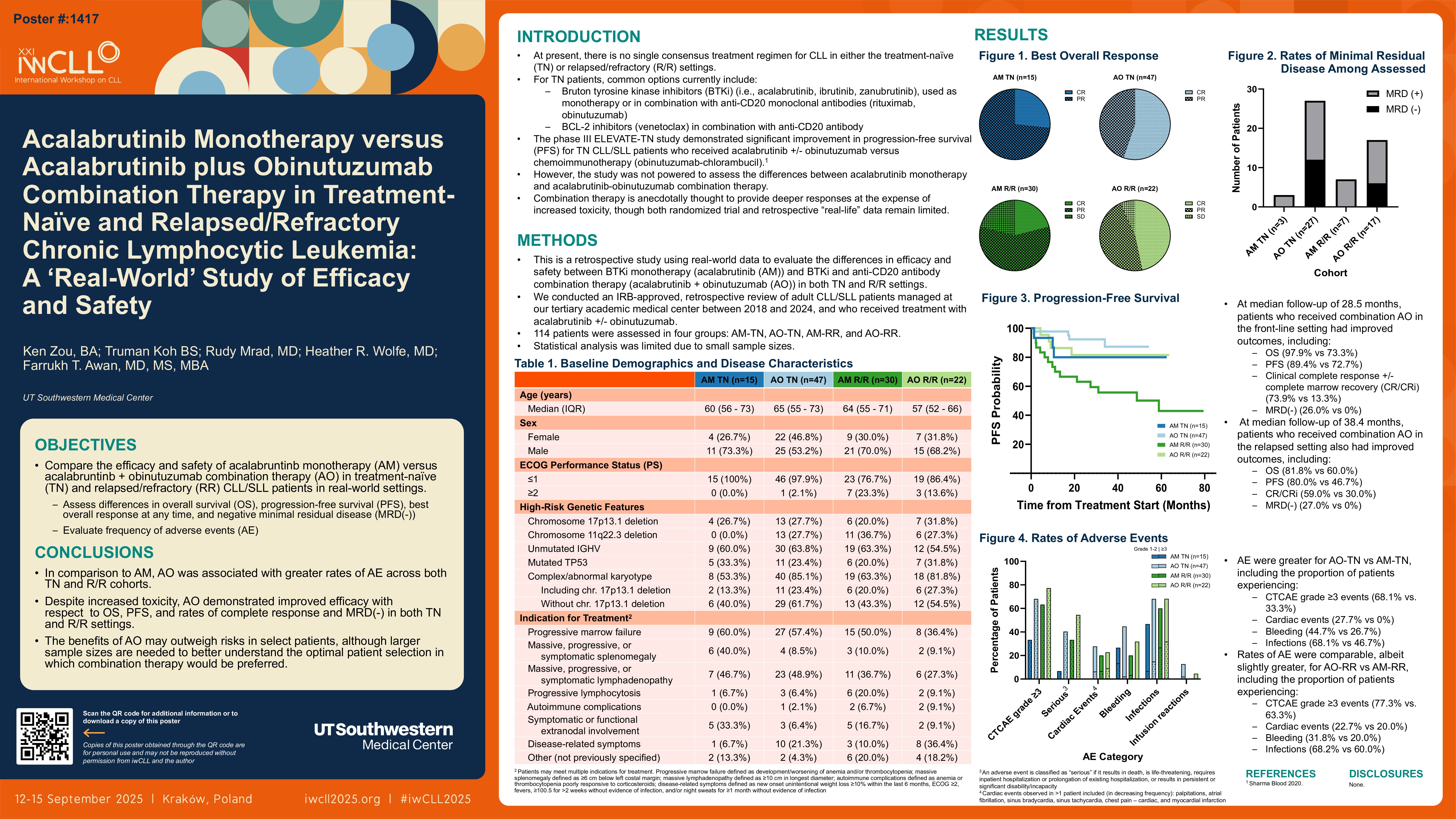
At present, there is no single consensus treatment regimen for CLL in either the treatment-naïve (TN) or relapsed/refractory (R/R) settings. For TN patients, common options currently include Bruton tyrosine kinase inhibitors (BTKi) (i.e., acalabrutinib, ibrutinib, zanubrutinib), which are used as monotherapy or in combination therapy with anti-CD20 monoclonal antibodies (rituximab or obinutuzumab), and/or BCL-2 inhibitors (venetoclax) in combination with anti-CD20 antibody. The phase III ELEVATE-TN study demonstrated significant improvement in progression-free survival (PFS) for TN CLL/SLL patients who received acalabrutinib +/- obinutuzumab versus chemoimmunotherapy (obinutuzumab-chlorambucil). However, the study was not powered to assess the differences between acalabrutinib monotherapy and acalabrutinib-obinutuzumab combination therapy. Combination therapy is anecdotally thought to provide deeper responses at the expense of increased toxicity, although both randomized trial and retrospective “real-life” data remain limited. This is a retrospective study using real-world data to evaluate the differences in efficacy and safety between BTKi and anti-CD20 antibody combination therapy (acalabrutinib + obinutuzumab (AO)) and BTKi monotherapy (acalabrutinib (AM)) in both TN and R/R settings.
Methods
We conducted an IRB-approved, retrospective review of adult CLL/SLL patients managed at our tertiary academic medical center between 2018 and 2024, and who received treatment with acalabrutinib +/- obinutuzumab. 114 patients were assessed in four groups – AO-TN (n=47), AM-TN (n=15), AO-RR (n=22), and AM-RR (n=30). Data was collected on patient demographics, baseline disease characteristics, treatment patterns, adverse events (AEs), and outcomes. Statistical analysis was limited due to small sample sizes.
Results
Treatment-Naive Cohorts
Baseline demographics and disease characteristics were similar between AO-TN and AM-TN for median age (65 vs 60 years), ECOG performance status ≤1 (97.9% vs 100%), and high-risk genetic features, including chromosome 17p13.1 deletion (27.7% vs 26.7%), unmutated IGHV (63.8% vs 60.0%), and TP53 mutation (23.4% vs 33.3%). Gender distribution was more balanced for AO-TN (46.8% female, 53.2% male) than AM-TN (26.7% female, 73.3% male). The most common treatment indication in both groups was progressive marrow failure (57.4% vs 60.0%). AEs were greater for AO-TN vs AM-TN, including the proportion of patients experiencing CTCAE grade ≥3 events (68.1% vs. 33.3%), cardiac events (27.7% vs 0%), bleeding (44.7% vs 26.7%), infections (68.1% vs 46.7%), and infusion-related reactions (12.8% vs 0%). With a median follow-up of 28.5 months, patients who received combination AO in the front-line setting had improved outcomes including improved overall survival (OS) (97.9% vs 73.3%), PFS (89.4% vs 72.7%), and rates of clinical complete response +/- complete marrow recovery (CR/CRi) (73.9% vs 13.3%), including higher rates of minimal residual disease negativity by flow cytometry (MRD(-)) (26.0% vs 0%).
Relapsed/Refractory Cohorts
Baseline demographics and disease characteristics were also similar between AO-RR and AM-RR for median age (57 vs 64 years), gender distribution (31.8% vs 30.0% female, 68.2% vs 70.0% male), ECOG performance status ≤1 (86.4% vs 76.7%), and high-risk genetic features, including chromosome 17p13.1 deletion (31.8% vs 20.0%), unmutated IGHV (54.5% vs 63.3%), and TP53 mutation (31.8% vs 20.0%). The most common treatment indication in both groups was progressive marrow failure (36.4% vs 50.0%). Rates of AEs were comparable, albeit slightly greater for AO-RR vs AM-RR, including the proportion of patients experiencing CTCAE grade ≥3 events (77.3% vs. 63.3%), cardiac events (22.7% vs 20.0%), bleeding (31.8% vs 20.0%), infections (68.2% vs 60.0%), and infusion-related reactions (4.5% vs 0%). With a median follow-up of 38.4 months, patients who received combination AO in the relapsed setting had improved outcomes, including improved OS (81.8% vs 60.0%), PFS (80.0% vs 46.7%), CR/CRi rates (59.0% vs 30.0%), and higher rates of MRD(-) (27.0% vs 0%).
Conclusions
Our results demonstrate that in both TN and R/R patients, AO was associated with an increased risk for AEs compared to AM. Nonetheless, combination therapy may offer a significant improvement across multiple outcome measures (i.e., OS, PFS, rates of CR/CRi and MRD(-)), which in some patients may outweigh the increased safety risks. In patients followed at specialized CLL treatment centers with robust coordination of care, AEs may be more rapidly triaged and managed, lending further support for the use of acalabrutinib + obinutuzumab combination therapy over acalabrutinib monotherapy alone. Larger sample sizes are needed to better understand the optimal patient population in which combination therapy would be preferred.
Keywords : BTKi combination therapy
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: