Authors
Michel van Gelder, Diderik-Jan Eikema, Joe Tuffnell, Linda Koster, Peter Dreger, Johannes Schetelig, Alexander Kulagin, Annoek Broers, Frédéric Baron, Nicolaus Kröger, Jan Vydra, Mi Kwon, Régis Peffault de Latour, Pavel Jindra, Tobias Gedde-Dahl, Ibrahim Yakoub-Agha, Carlos Solano Vercet, Martin Kaufmann, Edouard Forcade, Matthew Collin, Johan Maertens, Nicola Di Renzo, Joanna Drozd-Sokolowska, Kavita Raj, Donal P.McLornan, Olivier Tournilhac.
Introduction
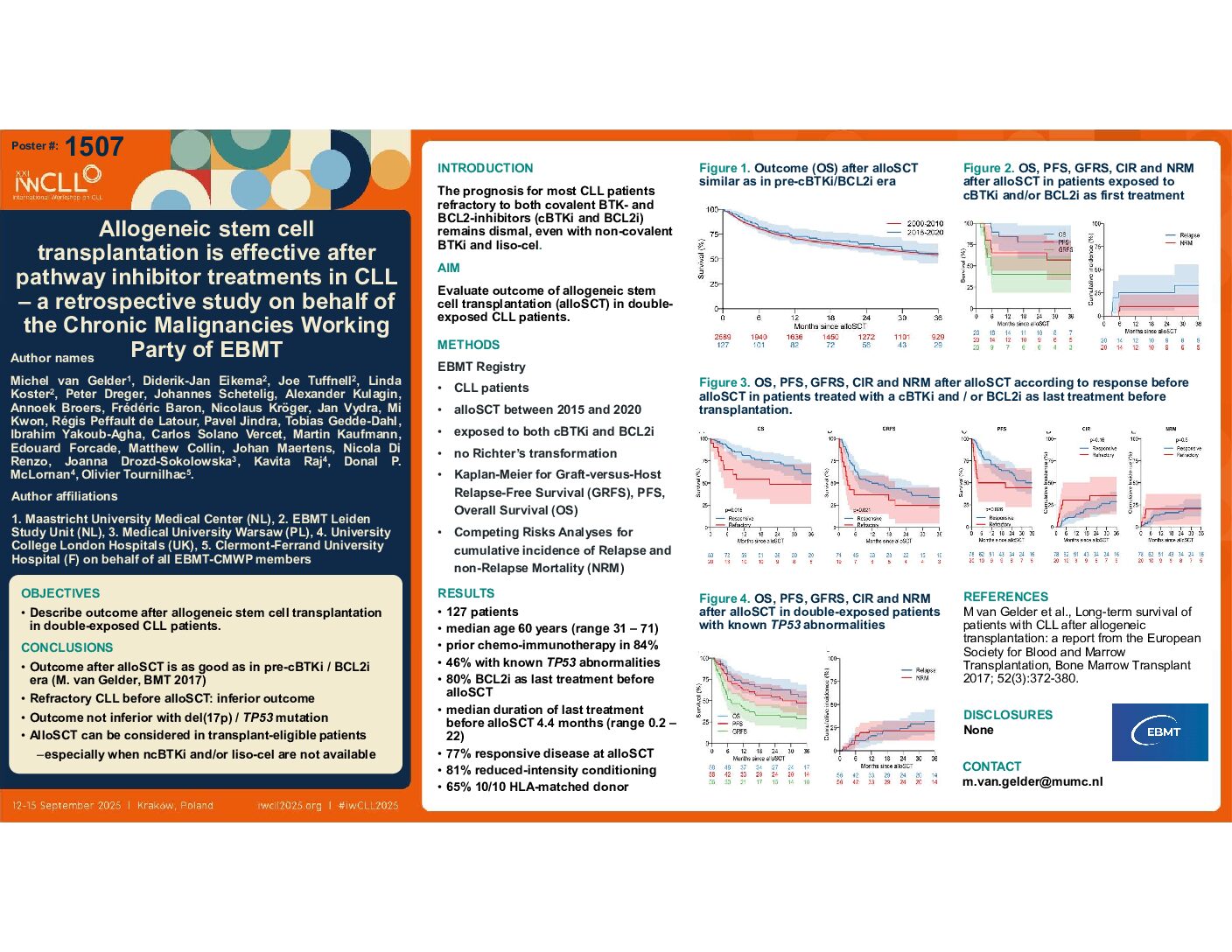
The life expectancy of CLL patients refractory to both BTK- and BCL2-inhibitors (BTKi & BCL2i) is dismal, even when non-covalent BTKi become available. We investigated if double-exposed patients may benefit from alloSCT.
Methods
From the EBMT Registry CLL patients were identified who had been exposed to both BTKi and BCL2i before alloSCT, excluding those with Richter’s transformation. The probabilities of Graft-versus-Host and Relapse-free survival (GRFS), Progression-free survival (PFS) and Overall Survival (OS) were calculated using the Kaplan-Meier method. Cumulative Incidence of Relapse and nonrelapse mortality (NRM) were analyzed as competing risks.
Results
We identified 127 patients, with a median age of 60 years (range 31-70). 78% had received chemotherapy before treatment with a BTKi and BCL2i, and 22 had also been treated with a PI3K-inhibitor (PI3Ki). Most patients (76%) were transplanted right after BCL2i treatment and only six after a PI3Ki. 76% were transplanted with responsive disease. The median follow-up of patients alive was 35 months.
There were 105 double-exposed patients, with a median age of 59 years. Their 3-year GRFS, PFS and OS were 30%, 48% and 56%, and 3-year Relapse Incidence and NRM were 30% and 21% respectively. For the 22 triple-exposed patients (median age 63 years), 3-year GRFS, PFS and OS were 20%, 36% and 56%, and 3-year Relapse Incidence and NRM were 34% and 30% respectively. Most NRM and relapse events occurred within 6 months after the transplantation.
3-year PFS for double- or triple exposed patients with responsive disease at transplant was 51% and 41%. Double-exposed patients with refractory disease at transplant had a 3-year PFS of 42%, while only one of the six triple-exposed refractory patients survived without progression.
There were 38 patients with known del(17p) and/or TP53 mutation, of whom 80% had been treated with chemotherapy before starting on a BTKi, BCL2i and, in six, on a PI3Ki. For 76% the last therapy before alloSCT was a BCL2i. 3-year GRFS, PFS and OS were 25%, 42% and 49%, and 3-year NRM and Relapse rate 22% and 35% respectively.
Conclusions
The median survival for double-exposed patients who subsequently underwent alloSCT exceeded three years, with a 3-year OS of 56%.
When relapse occurred, most cases were observed within six months after alloSCT. Non-relapse mortality (NRM) appears comparable to rates reported for CLL patients prior to the BTKi and BCL2i era (van Gelder et al., BMT 2017), where it was influenced by age. These results are favorable compared to those achieved with treatment using a non-covalent BTKi in double-exposed CLL patients. Finally, the optimal strategy remains unclear: whether to begin with a non-covalent BTKi before proceeding to alloSCT, or to perform alloSCT first and reserve non-covalent BTKi for use in relapsed patients.
Keywords : relapsed/refractory, allogeneic stem cell transplantation, TP53 anbormalities
Please indicate how this research was funded. : no direct funding, but unrestricted grants
Please indicate the name of the funding organization.: EBMT