Authors
A. Ferrario, G. Zamprogna, F. Perutelli, G. Camagni, L. Bertù, I. Innocenti, V. Oggianu, A. Cellini, M. Merli, R. Moia, F. Martini, A. Galitzia, E. Boccellato, F. De Falco, M. Deodato, E. A. Martino, M. Gentile, A. M. Frustaci, P. Sportoletti, L. Scarfò, G. Gaidano, C. Vitale, A. Visentin, R. Murru, L. Laurenti, M. Coscia.
Background
Among autoimmune complications, autoimmune cytopenias (AIC) involve 5-9% of patients affected by chronic lymphocytic leukemia (CLL), (Vitale C. et al, Cancers 2020). To date, the effects of acalabrutinib – a second-generation, covalent inhibitor of the BTK – on preexisting and treatment emergent AIC have not been fully investigated. In a few case reports, acalabrutinib has been successfully administered for the treatment of patients with immune thrombocytopenia (ITP) or pure red cell aplasia (PRCA), (Allsup D. et al. Leuk Lymphoma 2023; Fresa A. et al. Ther Adv in Hematology 2024). A phase II study evaluating the role of acalabrutinib in relapsed refractory autoimmune hemolytic anemia (AIHA) associated with CLL is currently ongoing.
Aims
The aim of this study is to analyze the characteristics and outcome of preexisting AIC and the incidence, features and outcome of treatment-emergent AIC in patients with CLL receiving acalabrutinib monotherapy.
Methods
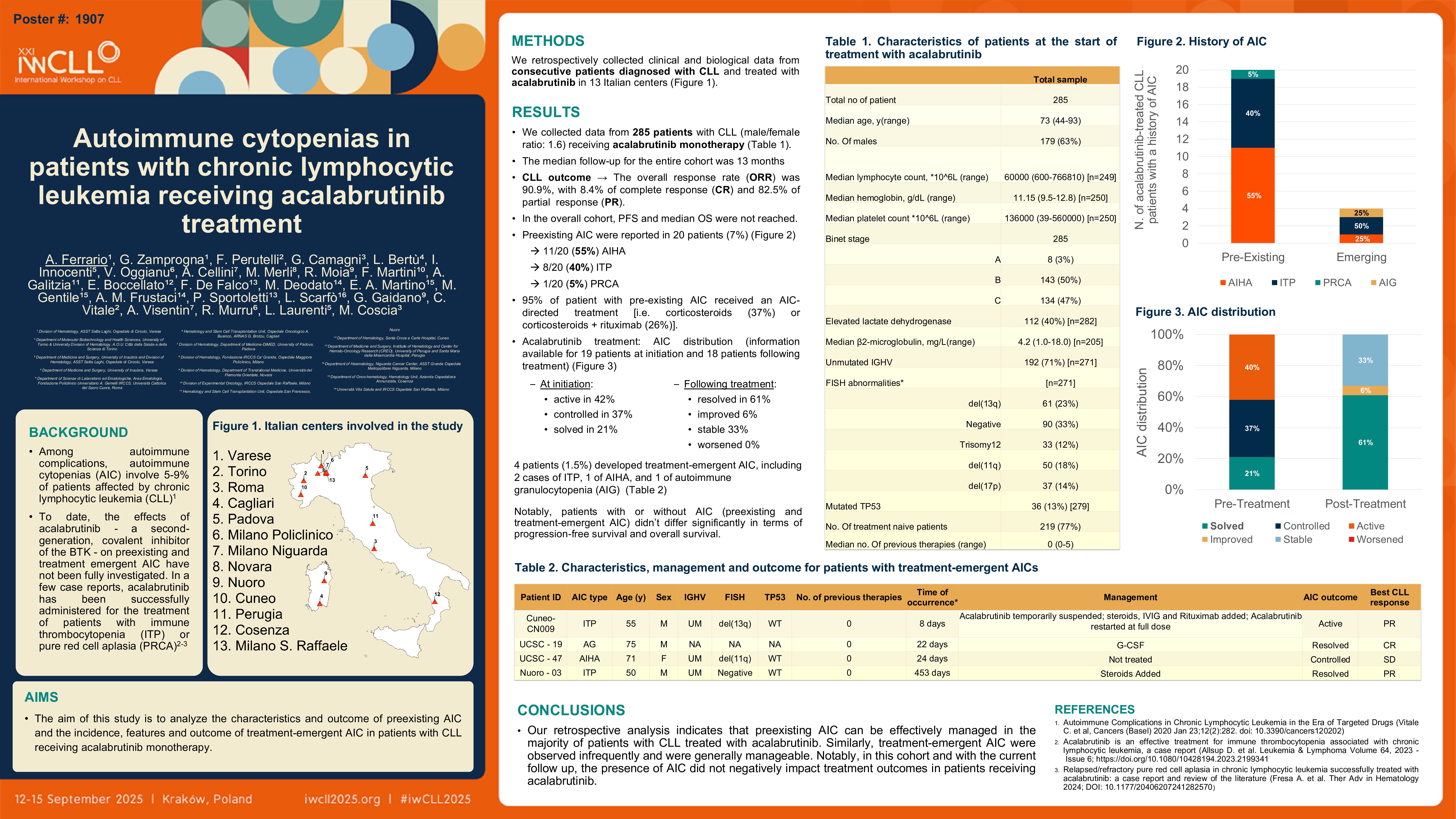
We retrospectively collected clinical and biological data from consecutive patients diagnosed with CLL and treated with acalabrutinib in 13 Italian centers.
Results
We collected data from 285 patients with CLL (male/female ratio: 1.6) receiving acalabrutinib treatment. The median age at treatment initiation was 73 years (range: 44–93), and the majority of patients (77%) were treatment-naïve. In our cohort, 192 of 271 patients (71%) harbored unmutated IGHV, 36/279 (13%) had TP53 mutations, and 37/271 (14%) carried del(17p). The median follow-up for the entire cohort was 13 months.
A history of AIC was present in 20 patients (7%), including 11/20 (55%) with AIHA, 8/20 (40%) with ITP, and 1/20 (5%) with PRCA. Nearly all patients with pre-existing AIC (95%) had received AIC-directed therapy, predominantly corticosteroids (37%) or corticosteroids combined with rituximab (26%). At the initiation of acalabrutinib treatment, AIC were active in 40%, controlled in 35%, and resolved in 20% of the patients. Following treatment with acalabrutinib, AIC resolved in 55% of cases and improved in an additional 5%.
In the entire cohort, 4 patients (1.5%) developed treatment-emergent AIC, including 2 cases of ITP, 1 of AIHA, and 1 of autoimmune granulocytopenia (AIG). Of the ITP cases, one achieved resolution with corticosteroids, while the second one required sequential therapy with corticosteroids, rituximab, intravenous immunoglobulin but failed to achieve control of the autoimmune complication thus requiring a temporary interruption of acalabrutinib. The patient with AIHA remained stable and did not require additional AIC-directed therapy. The case of AIG resolved with administration of granulocyte colony-stimulating factors (G-CSF). In terms of CLL outcome, patients with or without AIC – considering both preexisting and treatment-emergent AIC – did not differ significantly in terms of progression-free survival and overall survival.
Conclusions
Our retrospective analysis indicates that preexisting AIC can be effectively managed in the majority of patients with CLL treated with acalabrutinib. Similarly, treatment-emergent AIC were observed infrequently and were generally manageable. Notably, the presence of AIC did not negatively impact treatment outcomes in patients receiving acalabrutinib.
Keywords : Autoimmune cytopenias, chronic lymphocytic leukemia, acalabrutinib
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: