Authors
Marie Hodges PhD, Jared Darcy MRes, Rachel Bruton PhD, Thomas Roberts MSc, Wayne Croft PhD,Paul Moss MBBS, PhD, Matt Pugh MbChB PhD, Mohammed Nimir, MBChB Jonathan Cook PhD, Guy Pratt, MBBS, PhD, Shankara Paneesha MBBS MD, Naeem Khan PhD, Brian Willett PhD, Piers Patten MBChB, PhD, Talha Munir, MBBS, PhD, Andy Rawstron, PhD, Helen M. Parry, MBChB, PhD.
Background
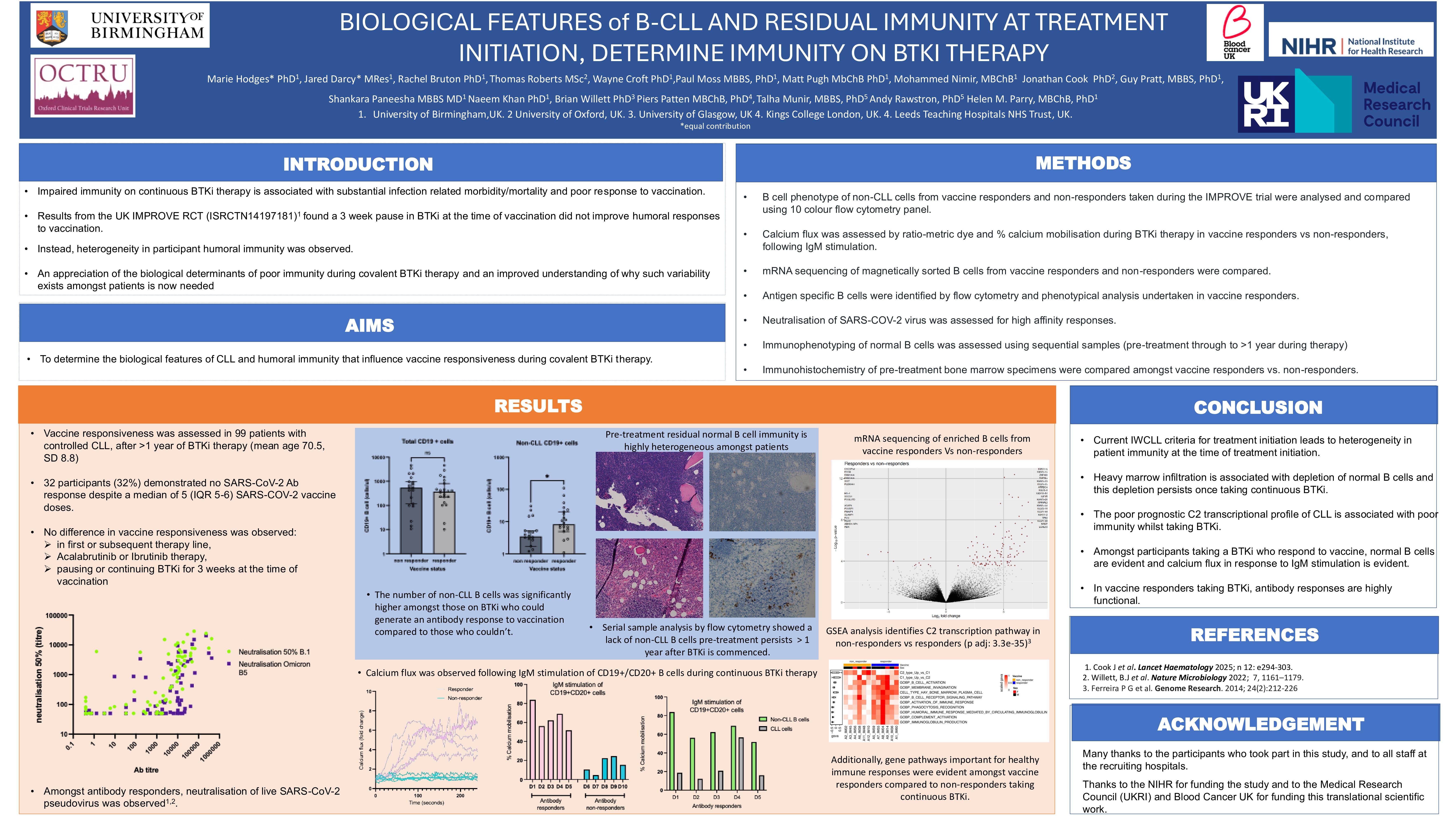
Impaired immunity on continuous BTKi therapy is associated with substantial infection related morbidity/mortality and poor response to vaccination in patients with CLL. The recently published UK IMPROVE Randomised control trial (ISRCTN14197181) investigated vaccine immunity for patients taking BTKi and reported heterogeneity in patient humoral immunity. An appreciation of the biological determinants of poor immunity during covalent BTKi therapy and an improved understanding of why such variability exists amongst patients, is now needed.
Aims
To determine the biological features of CLL and humoral immunity that influence infection risk and vaccine responsiveness during covalent BTKi therapy.
Methods
Using participant samples from IMPROVE, immunophenotyping of peripheral blood B cells was undertaken in vaccine responders versus non-responders to identify CLL and non-CLL B cell phenotype, followed by detection and phenotypic analysis of antigen-specific B cells amongst responders. Calcium flux analysis following IgM stimulation, along with mRNA sequencing of detectable B cells in antibody responders versus non-responders, was next investigated. An assessment of pre-treatment bone marrow samples by immunohistochemistry was also performed. Finally, serial immunophenotypic analysis of peripheral blood samples from therapy initiation to >1 year on BTKi were used to corroborate findings and the association with infection admission risk assessed.
Results
Of 99 patients with controlled CLL, following >1 year of BTKi therapy (mean age 70.5, SD 8.8), 32 participants (32%) demonstrated no SARS-CoV-2 Ab response despite a median of 5 (IQR 5-6) SARS-COV-2 vaccine doses. No difference in antibody titre was observed between: first or subsequent therapy line, acalabrutinib or ibrutinib therapy. Importantly, the number of non-CLL CD19+ B cells differed between responders (8.23 cells/ul (IQR 4.4-20.9)) and non-responders (3.4 cells/ul (IQR 1.4-5.2); p=0.02), with the greatest differences observed in IgM+ IgD+, CD27- naïve cells (responders:1.09 (IQR 0.3-3.1) Vs non-responders: 0.01(IQR 0-0.06) cells/ ul; p< 0.0001). Amongst antibody responders, B cell klickmers revealed a class switched IgG antigen-specific response and an intact calcium flux following BCR stimulation amongst non-CLL naïve B cells, despite continuous covalent BTK inhibition. Detectable CLL cells were evident in both responders and non-responders and no difference in total B cell number was observed (p=0.55). Non-responders strongly associated with a C2 transcription factor profile (p adj: 3.3e-35), whilst IGHV (unmutated Vs mutated) status did not. Immunohistochemistry and spatial transcriptomics demonstrated a heterogeneous degree of marrow infiltration by CLL at therapy initiation, contributing to the variability in normal B and plasma cell numbers. Serial analysis of peripheral immunophenotyping found the presence of normal B cells pretreatment impacts the B cell immune repertoire >1 year post therapy.
Summary/Conclusion
Current IWCLL criteria for treatment initiation leads to heterogeneity in patient immunity, with heavy marrow infiltration associated with the poor prognostic C2 transcriptional profile of CLL and impaired immunity. The depletion of naïve and memory B cells in pre-treatment work up, provides a tool for identifying those at risk of poor antigen-specific Ab responses during long term BTKi and may highlight individuals where antimicrobial prophylaxis may be beneficial.
Keywords : Immunity, leukaemia, BTKi
Please indicate how this research was funded. : Trial funding and Clinician Scientist funding for the laboratory work.
Please indicate the name of the funding organization.: UKRI (UK Research and Innovation), BCUK (Blood Cancer UK) and NIHR (National Institute for Health Research).