Central Nervous System Involvement in Patients with Richter Transformation (2MB pdf)
Authors
Domitilla Baccon, Paul J. Hampel, MD, Lindsey E. Roeker, MD, Saad S. Kenderian, MB, ChB, Eli Muchtar, MD Neil E. Kay, MD, Amber B. Koehler, PA-C, MS, Amy L. Behnken, APRN, CNP, MS, Catherine C. Wagner, APRN, CNP, DNP, Patrick B. Johnston, MD, PhD, Grzegorz S. Nowakowski, MD, Thomas M. Habermann, MD, Talal Hilal, MD2 Mazie Tsang, MD, Jose F. Leis, MD, PhD, Allison C. Rosenthal, DO, Ricardo D. Parrondo, MD, Han W. Tun, MD, Min Shi, MD, PhD, Rebecca L. King, MD, Rong He, MD, Sameer A. Parikh, MBBS, Yucai Wang, MD, PhD.
Introduction
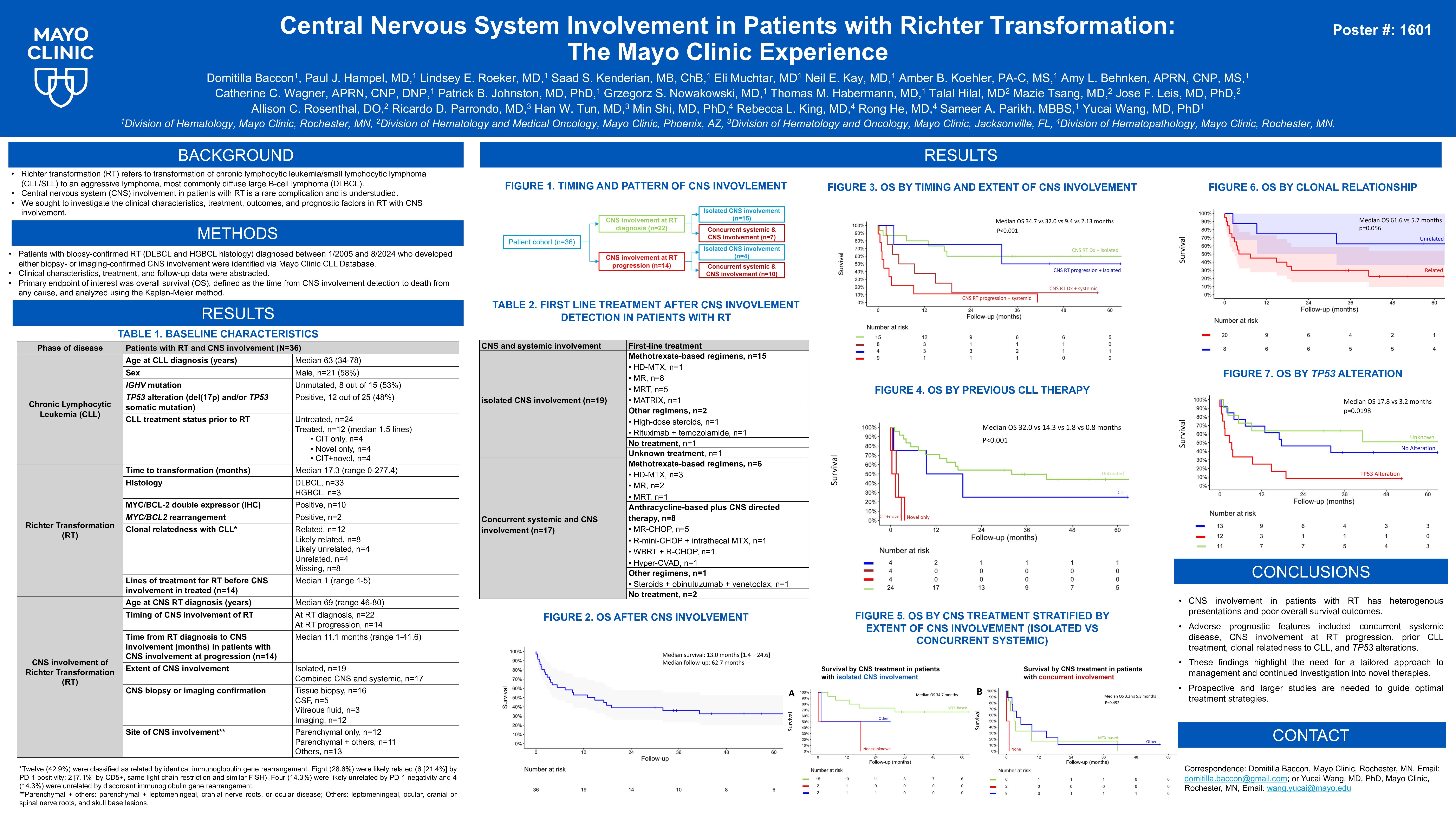
Central nervous system (CNS) involvement in patients with Richter transformation (RT) of chronic lymphocytic leukemia (CLL) is not well studied. This study aimed to describe clinical characteristics, treatment patterns, outcomes, and prognostic factors of CNS involvement in patients with RT seen at Mayo Clinic.
Methods
Patients with RT (diffuse large B-cell lymphoma [DLBCL] or high-grade B-cell lymphoma [HGBCL]) diagnosed between 1/2005 and 8/2024 who had CNS involvement were identified from the Mayo Clinic CLL Database and electronic health record. Clinical characteristics, treatment and follow-up data were abstracted. Overall survival (OS) was defined as time from CNS involvement detection to death from any cause and analyzed using the Kaplan-Meier method.
Results
A total of 36 patients with RT with documented CNS involvement were included: 24 with CNS biopsy confirmation and 12 with MRI evidence consistent with CNS involvement of biopsy-confirmed systemic RT.
The median age at CLL diagnosis was 63 years (range 34–78), and 21 (58%) patients were males. IGHV was unmutated in 8 of 15 (53.3%) patients with data available. CLL FISH results prior to or at RT diagnosis were available for 26 patients: 9 (34.6%) with del(17p), 6 (23.1%) with trisomy 12, 7 (26.9%) normal, and 4 (15.4%) with del(13q). Four of 11 (36.4%) patients had TP53 somatic mutation prior to or at RT diagnosis. The median time between CLL and RT diagnoses was 1.4 years (0–23.1). Prior to RT, 12 of 36 patients had received treatment for CLL (median lines of therapy 2 [range 1–5]), 5 with chemoimmunotherapy (CIT) alone, 5 with CIT and novel agents, and 2 with novel agents only.
The histology of RT was DLBCL in 33 patients and HGBCL in 3, including 2 MYC/BCL2 double-hit by FISH and 1 NOS. Thirteen (61.9%) had GCB subtype and 8 (38.1%) had non-GCB subtype by Hans algorithm (15 unknown). Ten (27.8%) had MYC/BCL2 double expression by IHC. Eight of 17 (47.1%) had PD-1 expression by IHC. Twenty of 28 (71.4%) exhibited clonal relatedness between CLL and RT.
Twenty-two patients had CNS involvement at RT diagnosis (15 with isolated CNS involvement and 7 with concurrent systemic and CNS involvement); the remaining 14 had received a median of 1 line of therapy (range 1–5) for RT before developing CNS involvement (4 with isolated CNS involvement and 10 with concurrent systemic and CNS involvement), with a median time from RT diagnosis to CNS involvement of 11.1 months (range 1–41.6). Predominant CNS involvement sites included parenchymal (n=24, 66.7%), leptomeningeal (n=9, 25.0%), and ocular or cranial/spinal root (n=3, 8.3%).
The first treatment for CNS involvement included high-dose methotrexate-based (n=25), other regimens (n=4), none (n=5) and unknown (n=2). The median OS following CNS involvement detection for all patients was 13.0 months (95% CI 1.4–24.6). Patients with isolated CNS involvement (n=19) had significantly better OS compared to those with concurrent CNS and systemic disease (n=17) (median OS 34.7 vs. 3.1 months; P< 0.001; Figure 1A). Similarly, patients who presented with CNS involvement at RT diagnosis (n=22) had longer OS than those who developed CNS involvement at RT progression (n=14) (median OS 18.4 vs. 3.6 months; P=0.023; Figure 1B). CLL treatment-naïve patients (n=24) had significantly longer OS compared to those with previous CLL treatment (n=12) (median OS 32.0 vs. 1.7 months; P< 0.001; Figure 1C). Patients with clonally unrelated RT (n=8) showed a trend towards better OS than those with clonally related RT (n=20) (median OS 61.6 vs. 5.7 months; P=0.056; Figure 1D). Moreover, patients without TP53 alterations (n=12) showed longer OS compared to those with TP53 alterations (n=13) (median OS 17.8 vs 3.2 months; P=0.019).
Conclusions
In this cohort of patients with RT who had CNS involvement, we found that CNS involvement at RT progression, concurrent CNS and systemic involvement, treatment exposure for CLL prior to RT, clonal relatedness between CLL and RT, and TP53 alterations were associated with poor OS after CNS involvement. Multicenter studies are needed to better define the incidence, clinical characteristics, molecular profile, optimal therapeutic strategies, and prognosis for CNS involvement in patients with RT, particularly in the era of novel agents.
Keywords : Chronic lymphocytic leukemia (CLL), central nervous system (CNS), Richter Transformation (RT)
Please indicate how this research was funded. : No funding.
Please indicate the name of the funding organization.: No funding.