Authors
Christoph Brey, Mirela Dzindo, Deyan Y. Yosifov, Christof Schneider, Kirsten Fischer, Petra Langerbeins, Barbara Eichhorst, Michael Hallek, Hartmut Döhner, Stephan Stilgenbauer, Eugen Tausch.
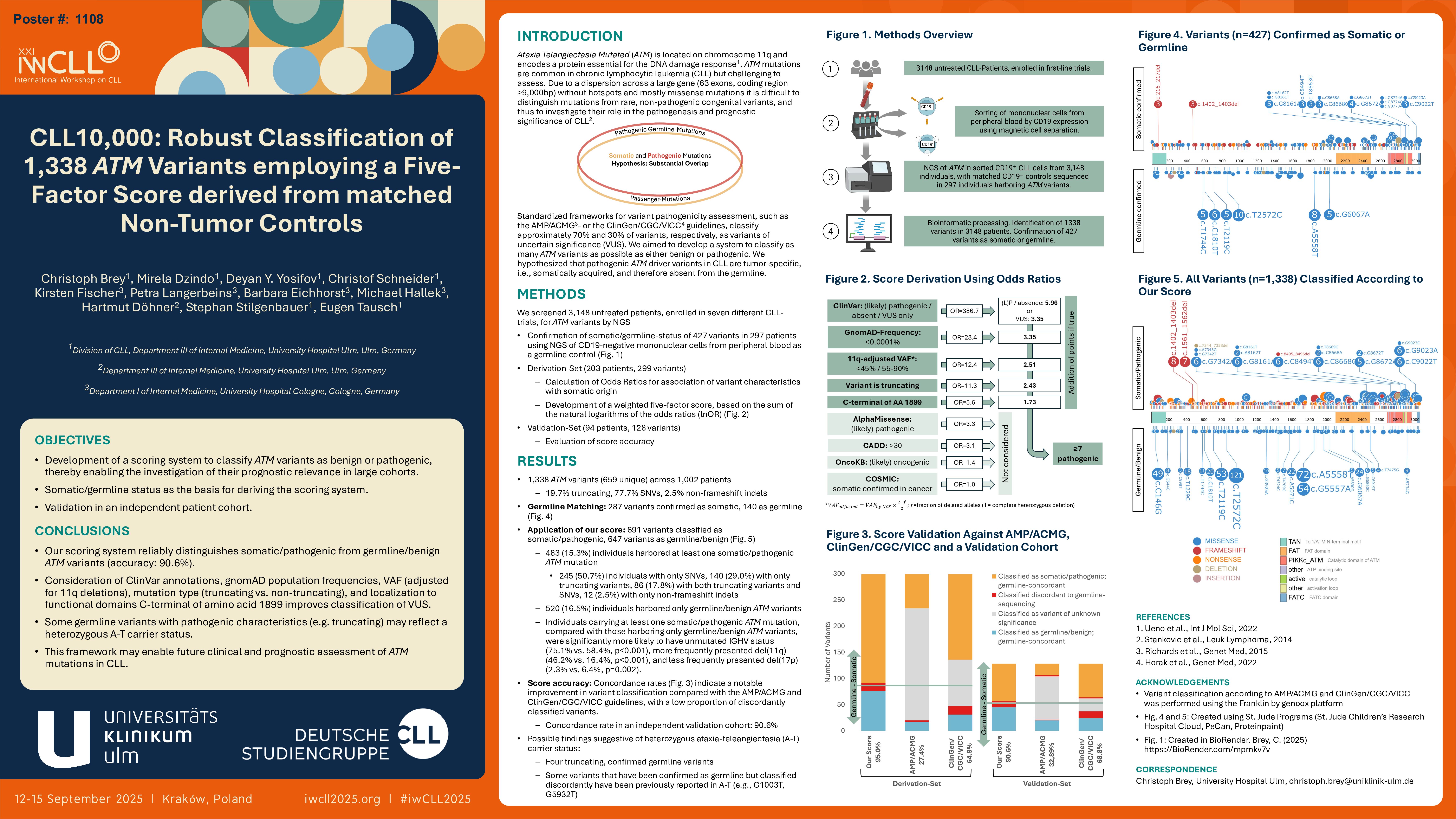
Mutations in ATM, an essential gene for DNA damage repair, are common in CLL but difficult to assess. Due to a dispersion across a large gene (63 exons, coding region >9,000 bp) without hotspots and mostly missense mutations it is difficult to distinguish mutations from rare, non-pathogenic congenital variants, and thus to investigate their role in the pathogenesis and prognostic significance of chronic lymphocytic leukemia (CLL).
To assess the incidence and co-factors of ATM mutations we screened 2829 untreated patients from five different CLL trials via Next Generation Sequencing (NGS). In total, we identified 1172 variants, of which 607 were unique, in 877 patients. Of these, 34.8% were truncating, 60.5% were nonsynonymous single-nucleotide variants (SNVs), and 4.8% were non-frameshift insertions or deletions.
Variant pathogenicity assessment employed standardized frameworks, including guidelines from the Association for Molecular Pathology (AMP) (Li et al., 2017) and the ClinGen/CGC/VICC consortium (Horak et al., 2022), to enable systematic evaluation. However, applying these gene-agnostic scores, a significant subset of variants – approximately 70% by AMP and 30% by ClinGen/CGC/VICC – were classified as variants of uncertain significance (VUS).
Based on the hypothesis that pathogenic ATM driver variants in CLL are tumor-specific, i.e. somatically acquired, and therefore absent from the germline, we sequenced matched non-tumor samples from 203 patients with ATM variants confirming 212 of the variants found in them as somatic/pathogenic and 87 as germline/benign. Factors associated with a somatic origin were amino acid position (AA >1898 corresponding to FAT/KD/FATC domain), mutation type (truncating), VAF adjusted for del(11q) (either at < 45% or 55-90%), gnomAD allele frequency ( < 1e-5), and ClinVar annotation (not listed or at least 1 classification as pathogenic); each showed strong concordance with their respective odds ratios (OR 5.6, 11.3, 12.4, 28.4, and 386.7), whereas listing of variants in the COSMIC database was not associated with somatic status. Therefore, we developed a weighted five-factor score based on the respective lnOR, ranging from 0 to 16. Variants scoring above the threshold of 7 were classified as somatic/pathogenic, while those below were considered germline/benign; importantly, the score was specifically designed to exclude uncertain significance (VUS) statuses due to their limited utility for statistical analysis in large cohorts.
Our score classified 284 of 299 variants (95.0%) in concordance with their somatic status as determined by comparison to germline. Overall, 15 variants (5.0%) were discordant with germline-matching results. However, since some variants that classified as somatic but were found in the germline have been previously reported in ataxia-telangiectasia (G1003T, G5932T), this finding may indicate a rare heterozygous A-T carrier status rather than a misclassification. Compared to the AMP guidelines (applied to our 299 variants: 27.4% concordance, 1.0% misclassification, 71.6% uncertain) and the ClinGen/CGC/VICC guidelines (64.9% concordance, 5.4% misclassification, 29.8% uncertain), our scoring system achieved a higher concordance rate (95%) and more accurately distinguished somatic from germline variants while minimizing misclassifications.
When applied to all 1,172 ATM mutations, 42.7% were classified as somatic/pathogenic by our score, including 38.8% nonsense, 56.9% missense, and 4.4% non-frameshift indel mutations. Among the 434 patients with somatic ATM mutations according to our scoring system, 73.7% exhibited an unmutated immunoglobulin heavy-chain variable (IGHV) status, 46.3% had a deletion at 11q22 [del(11q22)], and only 1.4% presented with a deletion at 17p13 [del(17p13)]. In contrast, among the 443 patients carrying exclusively ATM variants that were classified as germline/benign, 56.0% displayed an unmutated IGHV status, 15.6% harbored del(11q22), and 3.4% exhibited del(17p13).
We herein present a scoring system that reliably identifies pathogenic ATM variants and may facilitate the investigation of their prognostic impact in CLL across large cohorts. Independent validation will be performed in an additional patient cohort with matched non-tumor controls. In parallel, efforts will be made to complete the genetic landscape of ATM mutations and to assess the co-occurrence of other relevant markers. Associations with specific clinical and molecular factors will also be investigated.
Keywords : CLL, ATM, biomarker, genetics
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: