Authors
Surita Dalal, Jane Shingles, Sean Girvan, David Cairns, Nichola Webster, Andrew Rawstron, Darren Newton, Sue Bell, Natasha Greatorex, Anna Hockaday, Sharon Jackson, David Phillips, David Stones, David Allsup, Adrian Bloor, Anita Sarma, Abraham Varghese, Peter Hillmen and Talha Munir.
Introduction
Determination of the immunoglobulin heavy variable (IGHV) gene somatic hypermutation (SHM) status remains an important and independent prognostic marker in CLL. Additionally, in approximately one third of CLL the B-cell receptor (BcR) immunoglobulins (IG) display highly homologous variable heavy complementarity-determining region 3 (VH CDR3), and can be assigned to distinct subsets, with virtually identical or stereotyped BcR IG. Of the major subsets described, CLL subset #2 is the largest stereotyped subset (Agathangelidis et al, Blood. 2012). Present in CLL using the IGHV3-21 gene, this subset is characterised by poor clinical outcome, irrespective of SHM status (Baliakas et al, Blood. 2015). Stereotyped CLL subset #8, defined by the use of the IGHV4-39 gene, is associated with clinically aggressive disease and high risk of Richter’s transformation (RT) (Rossi et al, Hematol Oncol. 2009). Compared to chemoimmunotherapy, numerous trials using targeted treatment strategies with Ibrutinib (I) an irreversible Btk inhibitor, and Venetoclax (V), a Bcl-2 inhibitor have shown improved outcomes in CLL. FLAIR has reported improved Progression-Free Survival (PFS) and Overall Survival with MRD defined I+V compared to Fludarabine, Cyclophosphamide and Rituximab (FCR) in CLL (Munir et al, N Engl J Med. 2024). However, little is known regarding the synergistic effect of I+V on the response of subset #2 and #8 patients.
In this study we have investigated the 5-year PFS of CLL subset #2 patients comparing MRD defined I+V to the Ibrutinib (I alone and IR) and FCR arms of FLAIR. We also report on RT in FLAIR including CLL subset #8 patients.
Methods
FLAIR (ISRCTN01844152) is an ongoing phase III, multicentre, randomised, controlled, open-label trial in previously untreated CLL patients, comparing IR with FCR. It was subsequently adapted in July 2017 to compare I+V and I alone with FCR. Somatic hypermutation status was determined by PCR amplification of IGHV-IGHD-IGHJ gene rearrangements using IGHV leader/FR1 primers. Bidirectional Sanger sequencing was analysed using IMGT/V-Quest and the ARResT/AssignSubsets tool.
Results
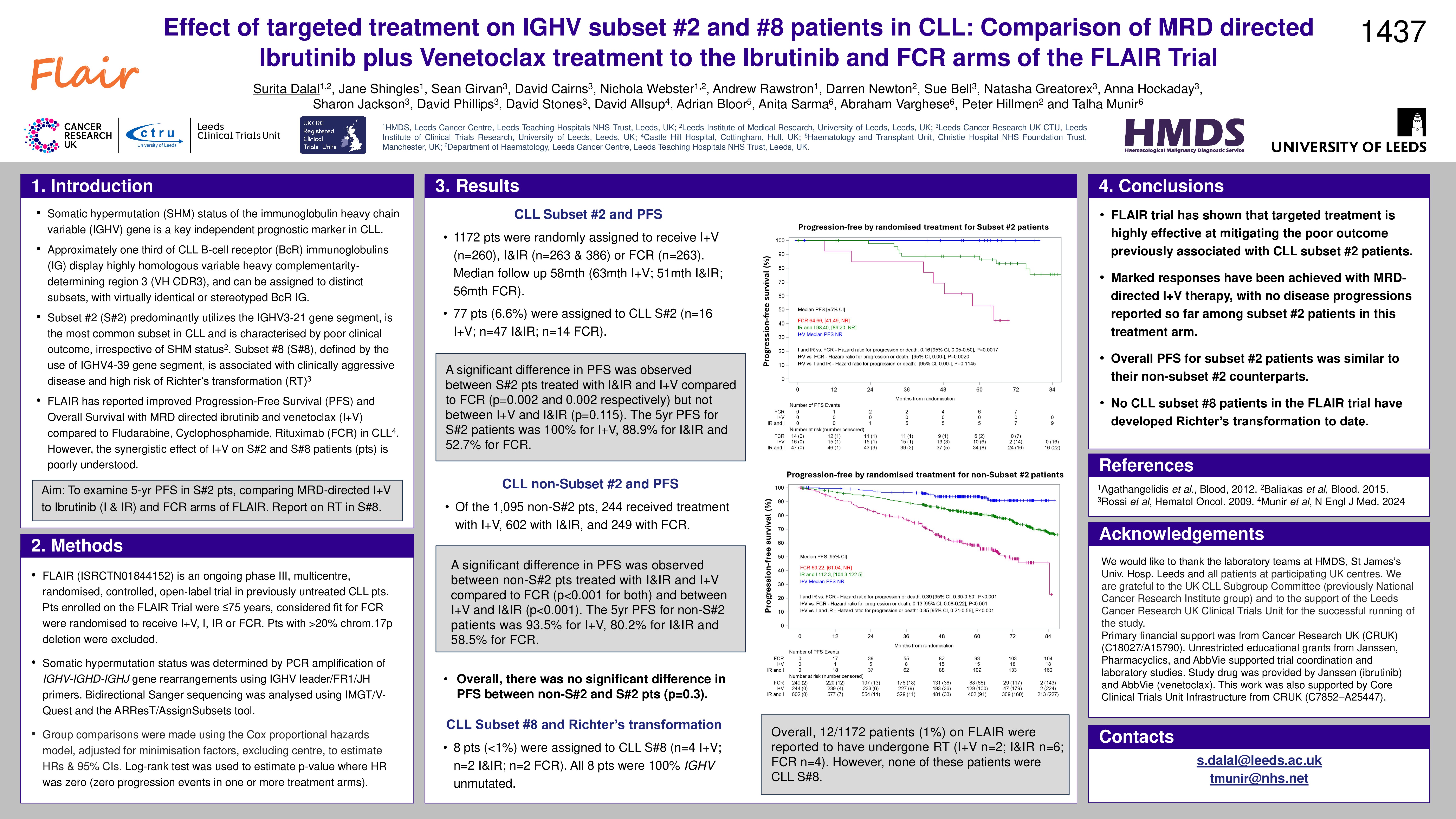
Of the 1172 patients included in this study, 79 patients were assigned to CLL subset #2 (6.7%). Of these 16 were treated with I+V, 49 with ibrutinib based therapies (I alone & IR arms combined) and 14 with FCR, with a median follow up of 58 months (63, 51 and 56 months respectively). Using Log-rank test, a significant difference in PFS was observed between subset #2 patients treated with I&IR and I+V compared to FCR (p=0.003 and 0.002 respectively) but not between I+V and I&IR (p=0.1873). The 5yr PFS for subset #2 patients was 100% for I+V, 88.9% for I&IR and 52.7% for FCR. Using Cox’s proportional hazards, a significant difference in PFS was also present between I&IR and I+V compared to FCR for non-subset #2 patients (HR:0.41 p< 0.001 and HR:0.13 p< 0.001 respectively). Additionally, the difference in PFS between I+V and I&IR was also significant (HR:0.32 p< 0.001). The 5yr PFS for non-subset #2 patients was 93.5% for I+V, 80.2% for I&IR and 58.5% for FCR. Overall, there was no significant difference in PFS between non-subset #2 patients and subset#2 patients (p=0.3).
Overall, 12/1172 patients (1%) on FLAIR were reported to have undergone RT (I+V n=2; I&IR n=6; FCR n=4). However, none of these patients were stereotyped CLL subset #8.
Conclusion
Flair trial has shown that targeted treatment is highly effective at mitigating the poor outcome previously associated with CLL subset #2 patients, with exceptional responses seen following MRD defined I+V treatment. To date none of the CLL subset #8 patients on FLAIR have undergone RT.
Keywords : FLAIR, IGHV, Subset#2
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: