Authors
Anita Soboń, Elżbieta Iskierka-Jażdżewska, Joanna Drozd-Sokołowska, Anna Puła, Małgorzata Gajewska, Michał Danecki, Łukasz Bołkun, Agata Ogłoza, Marta Morawska, Janusz Halka, Edyta Subocz, Agnieszka Podgórska, Jagoda Tryc-Szponder, Ewa Paszkiewicz-Kozik, Anna Kopińska, Justyna Rybka, Agnieszka Szymczyk, Kamil Wdowiak, Paweł Steckiewicz, Iwona Hus, Krzysztof Jamroziak, Tadeusz Robak, Ewa Lech-Marańda and Bartosz Puła.
Background
The prognosis of patients with relapsed/refractory chronic lymphocytic leukemia (RR-CLL) has improved following the introduction of venetoclax into clinical practice. In the MURANO trial, RR-CLL patients treated with venetoclax and rituximab (VEN-R) experienced significantly longer progression-free survival (PFS) and overall survival (OS) compared to those treated with bendamustine and rituximab (BR). Since then, this regimen has become firmly established in the standard therapeutic landscape for RR-CLL and is widely used in clinical practice.
Aims
To assess the clinical efficacy and safety profile of VEN-R treatment in patients with RR-CLL outside of clinical trials.
Methods
We conducted a retrospective analysis of RR-CLL patients treated with VEN-R at hematology centers affiliated with the Polish Adult Leukemia Study Group (PALG) between 2019 and 2024.
Results
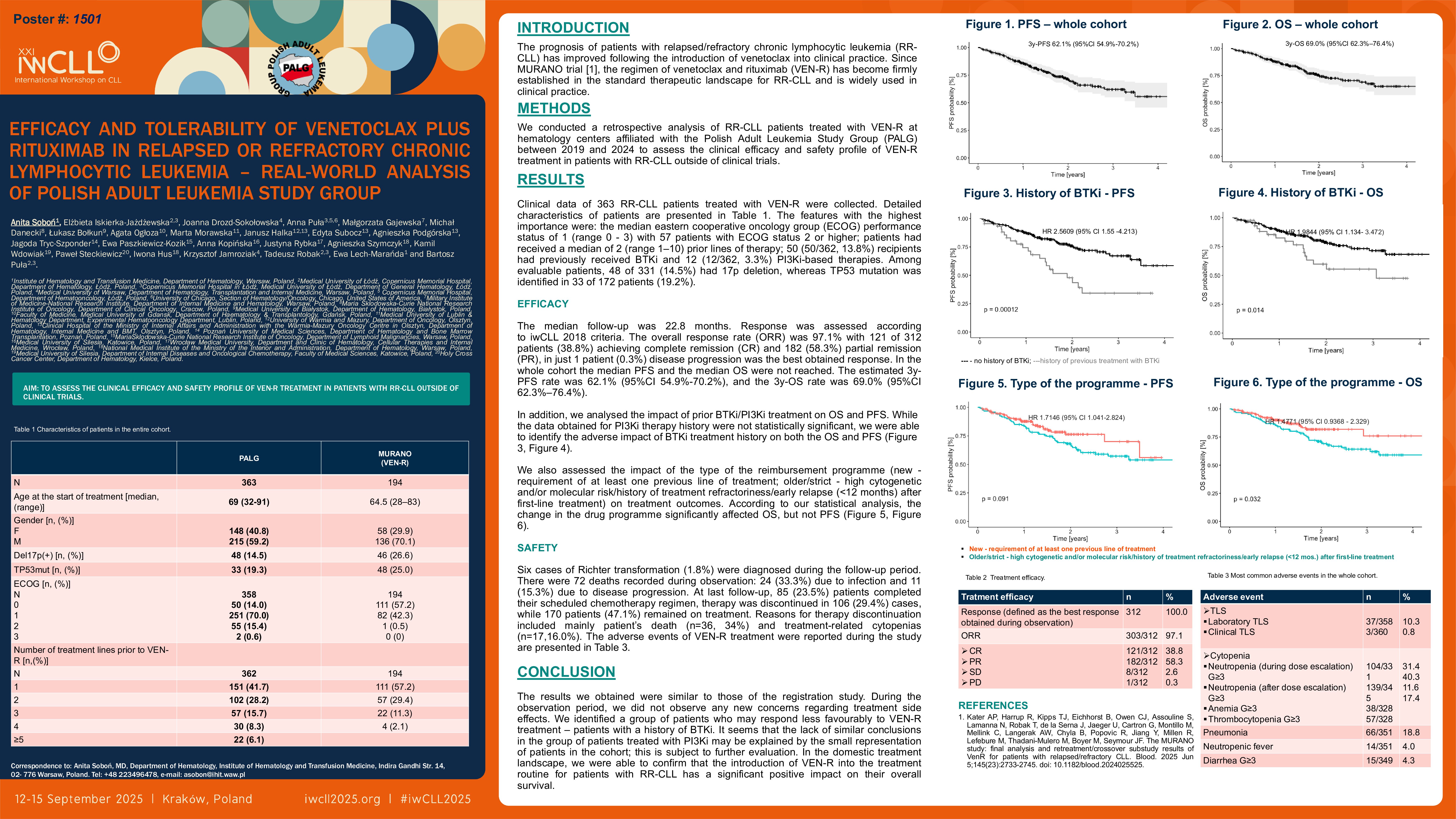
Clinical data of 363 RR-CLL patients treated with VEN-R were collected. The median age at initiation of VEN-R therapy was 69 years (range 32 – 91 years), and 215 patients (59.2%) were male. The median Cumulative Illness Rating Scale (CIRS) was 6 (range 0 – 19) and the median Eastern Cooperative Oncology Group (ECOG) performance status was 1 (range 0 – 3) with 57 (57/358, 15.9%) patients with ECOG status 2 or higher. Patients had received a median of 2 (range 1–10) prior lines of therapy, whereas 151 patients (41.6%) had relapsed after first-line treatment. 52 (52/363, 14.3%) recipients had previously received BTKi or 12 (12/362, 3.3%) PI3Ki-based therapies. Among evaluable patients, 48 of 331 (14.5%) had 17p deletion, whereas TP53 mutation was identified in 33 of 172 patients (19.2%). The median follow-up was 22.8 months. Response was assessed according to iwCLL 2018 criteria. The overall response rate (ORR) was 97.1% with 121 of 312 patients (38.8%) achieving complete remission (CR), 182 (58.3%) partial remission (PR), and 1 patient (0.3%) showing disease progression at the best response. Among patients with TP53 mutation, CR and PR were observed in 30 (90.9%), SD in 2 (6.1%), and the response was not assessed in one patient. Among patients with 17p deletion, 39 (81.3%) achieved CR or PR, 3 (6.3%) achieved SD, and the response was not assessed in six patients. In the whole cohort the median PFS and the median OS were not reached. The estimated 3y-PFS rate was 62.1% (95%CI 54.9-70.2), and the 3y-OS rate was 69.0% (95%CI 62.3–76.4). Six cases of Richter transformation (1.8%) were diagnosed during the follow-up period. There were 72 deaths recorded during observation: 24 (33.3%) due to infection and 11 (15.3%) due to disease progression. At last follow-up, 85 (23.5%) patients completed their scheduled chemotherapy regimen, therapy was discontinued in 106 (29.4%) cases, while 170 patients (47.1%) remained on treatment. Reasons for therapy discontinuation included mainly patient’s death (n=36, 34%) and treatment-related cytopenias (n=17,16.0%). The following adverse events of VEN-R treatment were reported during the study: all grade neutropenia during dose escalation (223/331, 67.4%, with grade 3/4 in 104/331 patients, 31.4%) and after dose escalation period (276/345, 80%, with grade 3/4 in 139/345, 40.3% of all neutropenia). Other adverse effects observed independently of treatment phase were: anemia (grade 3/4 in 38/328, 11.6%), thrombocytopenia (grade 3/4 in 57/328, 17.4%), pneumonia (66/351, 18.8%), neutropenic fever (14/351, 4.0%), diarrhea (15/349, 4.3%), autoimmune hemolytic anemia (8/346, 2.3%) and immune thrombocytopenic purpura (8/344, 2.3%) and in one case exacerbation of heart failure was observed.
Summary/Conclusion
In this retrospective analysis, the outcomes of treatment with the VEN-R regimen in a real-life setting were slightly worse as compared to the results of the MURANO trial, probably due to the inclusion of a higher number of patients with advanced ECOG and more heavily pretreated, including BTK inhibitors.
Keywords : Venetoclax, relapsed/refractory CLL, real-world data
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: