Authors
Anna Oh, PhD, MPH, RN1,, Justin Abuel, BS, Briana Williams, BS, Alfonso Molina, MD, MPH, Michael Conte, PA-C, Gabriel Mannis, MD, William Shomali, MD, Michaela Liedtke, MD, Jason Gotlib, MD, Beverly Mitchell, MD, Tait Shanafelt, MD, Bita Fakhri, MD, MPH.
Introduction
Chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL) are related B-cell malignancies that represent the most common form of adult leukemia. Although clinical trials are crucial in advancing novel therapeutic options, unequal participation based on sociodemographic factors can limit the generalizability of trial findings to a broader patient population. This project assessed the demographic characteristics of CLL/SLL clinical trial participants at a large National Cancer Institute (NCI)-designated Cancer Center in Northern California (2012-2024) and compared these characteristics with national and regional disease prevalence estimates from the NCI’s Surveillance, Epidemiology, and End Results (SEER) database.
Methods
We conducted a retrospective analysis of all interventional trials involving adults aged 18 years and older with CLL/SLL at the Stanford Cancer Institute from 2012 to 2024, utilizing institutional databases. Demographic data, including age, sex, race/ethnicity, preferred language, insurance status, and residential ZIP code, were extracted from electronic medical records.
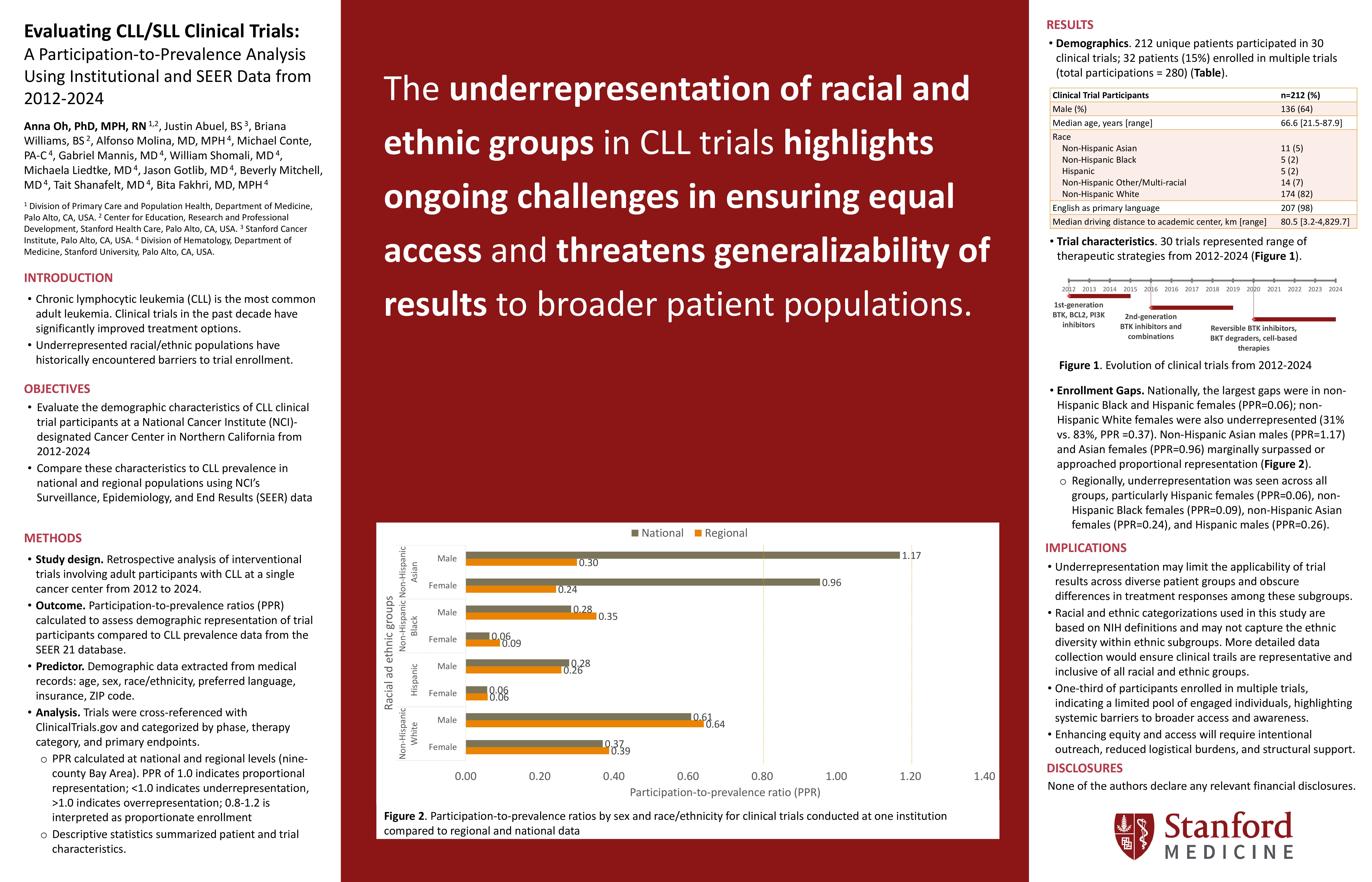
The trials were cross-referenced with ClinicalTrials.gov and categorized based on study phase, intervention class (including BTK inhibitors, PI3K inhibitors, BCL2 inhibitors, and cell-based therapies), and primary outcomes. To assess the representation of trial participants, we calculated participation-to-prevalence ratios (PPR) by comparing the demographics of trial participants with the prevalence data from the SEER 21 database, both nationally and within the nine-county Bay Area, which serves as our institution’s catchment area. A PPR of 1.0 indicates proportional representation, a PPR of less than 1.0 indicates underrepresentation, and a PPR greater than 1.0 indicates overrepresentation. Descriptive statistics were employed to summarize patient and trial characteristics, providing a comprehensive overview of the demographic landscape of CLL/SLL clinical trial participants in relation to the broader population affected by these malignancies.
Results
A total of 212 unique patients enrolled in 30 different clinical trials for CLL/SLL between 2012-2024, contributing to 280 trial participations. Median age at first enrollment was 66.6 years (range: 21.5-87.9); 64% identified as male. The racial/ethnic distribution included: 5% non-Hispanic Asian, 2% non-Hispanic Black, 2% Hispanic, 7% non-Hispanic other/multiple groups, 2% unknown, and 82% non-Hispanic White; 98% reported English as their primary language. Insurance coverage was primarily Medicare (54%), private insurance (22%), and managed care (20%). Most trial participants (54%) resided in the Bay Area, with median driving distance of 80.5 kilometers (range: 3.2-4,829.7).
Of the 212 participants, 68 (32%) enrolled in multiple trials. The highest number of trial enrollments observed was two individuals who participated in four trials. The 30 trials represented a range of therapeutic strategies. Trials between 2012-2014 involved first-generation BTK, BCL2, or PI3K inhibitors, either as monotherapy or combined with immunotherapy. From 2015-2019, trials evaluated second-generation BTK inhibitors and additional BTK and BCL2 inhibitor combinations. Since 2020, studies have focused on reversible BTK inhibitors, BTK degraders, and cell-based therapies. Eighteen trials (60%) targeted relapsed/refractory disease, while 11 (37%) targeted treatment-naïve populations. The most common endpoints were progression-free survival (47%), safety or tolerability (30%) and overall response rate (27%).
Compared with national SEER prevalence data, observed trial enrollment was not reflective of CLL/SLL prevalence in most sex and racial/ethnic groups. The largest gaps in enrollment were among non-Hispanic Black and Hispanic females (both PPR=0.06, proportions not reported due to n < 5). Non-Hispanic White females were also enrolled at a lower rate (31% vs. 83%, PPR=0.37) compared to non-Hispanic White males (52% vs. 84%, PPR=0.61). Non-Hispanic Asian males (3% vs. 2%, PPR=1.17) and Asian females (2% vs. 3%, PPR=0.96) were the only groups with participation rates similar to population prevalence. Regionally, all groups showed lower representation, with the lowest PPRs among Hispanic females (0.06), non-Hispanic Black females (0.09), non-Hispanic Asian females (0.24), and Hispanic males (0.26).
Conclusion
Despite increased clinical trial activity in CLL/SLL, our institution’s clinical trial participants did not consistently reflect the sex and racial/ethnic profile of national and regional CLL/SLL populations. PPRs ranged from 0.06 to 1.17, with representation differing across sex and racial/ethnic categories relative to disease prevalence. These findings underscore a persistent gap in equitable representation and suggest that systemic barriers continue to limit access to trials for diverse populations, even within high-volume, research-intensive cancer centers. Future efforts should prioritize targeted outreach within institutional catchment areas, inclusive trial design, and strategies to address logistical and sociocultural barriers to enrollment, thereby enhancing clinical trial equity and generalizability of results.
Keywords : CLL/SLL; Clinical Trial Enrollment; Patient Representation
Please indicate how this research was funded. : No funding from external sources.
Please indicate the name of the funding organization.: N/A