Authors
Yost, A., Annamalay, A., Forsyth, C., Garcia Gonzalez, I., Ong, M., Scheepers, C., Venkatesh, V., Schuh, A., Garcia-Gonzalez, P.
Introduction
Chronic lymphocytic leukemia (CLL) is the most common leukemia in adults, accounting for approximately one third of new leukemia cases worldwide (Yao Y, et al., 2022). In low- and middle-income countries (LMICs), cancer incidence and mortality are rapidly increasing, yet access to targeted therapies and key diagnostic tools remains limited. To address this inequity, The Max Foundation (Max) in partnership with local health care providers (HCPs), global key opinion leaders from the International Workshop on CLL (iwCLL), and a biotechnology donor, launched a treatment access program to provide zanubrutinib, a second-generation BTK inhibitor (BTKi), at no cost to patients. To inform program implementation, a comprehensive institutional capacity assessment was conducted across potential partner institutions. The goal was to evaluate readiness to diagnose and treat CLL, identify resource gaps, and inform program planning.
Methods
A standardized capacity assessment tool was distributed to partner institutions in eligible countries. The tool collected quantitative and qualitative data across several domains, including annual CLL patient volume, clinical staffing, availability of diagnostic and prognostic services, access to CLL treatments, and presence of local cancer advocacy organizations. Preliminary analysis explored correlations between site capacity indicators and reported annual CLL patient volume using a Spearman’s correlation. Descriptive analysis identified trends, capacity, and key gaps in readiness.
Results
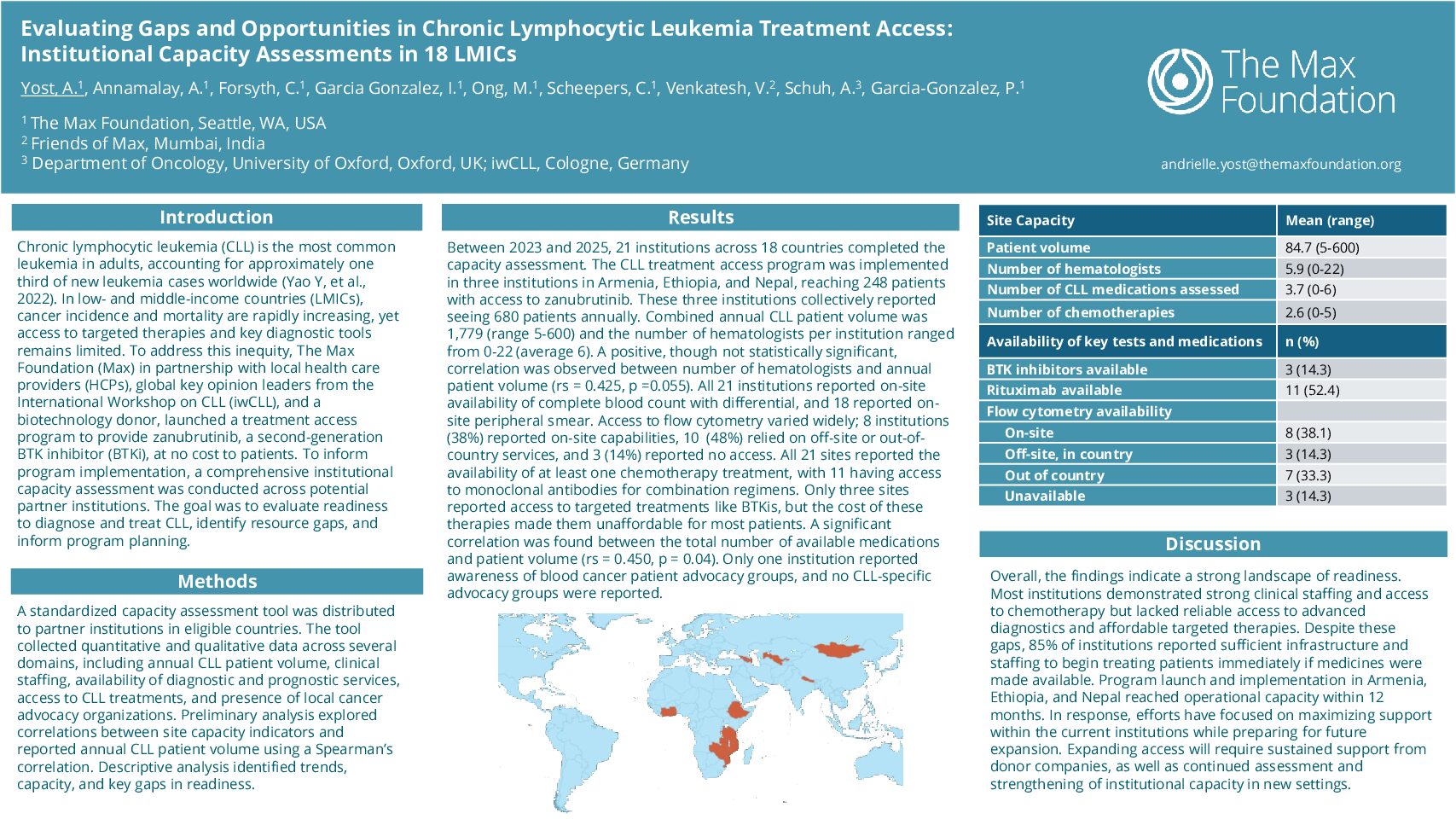
Between 2023 and 2025, 21 institutions across 18 countries completed the capacity assessment. The CLL treatment access program was implemented in three institutions in Armenia, Ethiopia, and Nepal, reaching 248 patients with access to zanubrutinib. These three institutions collectively reported seeing 680 patients annually. Across all 21 institutions, the total reported annual CLL patient volume was 1,779 (range 5-600) and the number of hematologists per institution ranged from 0-22 (average 6). A positive, though not statistically significant, correlation was observed between number of hematologists and annual patient volume (rs = 0.425, p =0.055). All 21 institutions reported on-site availability of complete blood count with differential, and 18 institutions reported on-site peripheral smear capabilities. However, access to flow cytometry, the gold standard diagnostic for CLL diagnosis, varied widely; 8 institutions (38%) reported on-site capabilities, 10 institutions (48%) relied on off-site or out-of-country services, and 3 institutions (14%) reported no access to flow cytometry. All 21 sites reported the availability of at least one chemotherapy treatment, with 11 having access to monoclonal antibodies for combination regimens. Only three sites reported access to targeted treatments like BTKis, but the cost of these therapies made them unaffordable for most patients. A significant correlation was found between the total number of available medications and patient volume (rs = 0.450, p = 0.04). Only one institution reported awareness of blood cancer patient advocacy groups, and no CLL-specific advocacy groups were reported.
Discussion
Overall, the findings indicate a strong landscape of readiness. Most institutions demonstrated strong clinical staffing and access to chemotherapy but lacked reliable access to advanced diagnostics and affordable targeted therapies. Despite these gaps, 85% of institutions reported sufficient infrastructure and staffing to begin treating patients immediately if medicines were made available. Program launch and implementation in Armenia, Ethiopia, and Nepal reached operational capacity within 12 months. In response, efforts have focused on maximizing support within the current institutions while preparing for future expansion. Expanding access will require sustained support from donor companies, as well as continued assessment and strengthening of institutional capacity in new settings.
Keywords : LMIC, treatment access, Bruton’s tyrosine kinase inhibitor (BTKi)
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: