Authors
Agnieszka Giza, Jan Novak, Paolo Ghia, Jacqueline Barrientos, Mitul Gandhi, Mark Hoffman, Brian Koffman, Christopher Abbazio, Erin Franceschini, Ping Xu, Brooke Patterson, Christoph Tapprich, Claire Kavanagh, Sowmya Srikanthan, Bothayna Messahel, Wasiulla Khan, Tadeusz Robak.
Background
Ibrutinib monotherapy or in combination with venetoclax (I+V) has dramatically changed the treatment landscape for patients with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), providing overall survival comparable with that of an age-matched general population. Ten-year follow-up data from the RESONATE-2 study showed robust long-term efficacy of continuous ibrutinib monotherapy in previously untreated CLL/SLL. Fixed-duration (FD) I+V demonstrated clinical benefit with deep and durable responses in the GLOW and CAPTIVATE studies. Considering disease heterogeneity and other factors that influence treatment decisions, an unmet need exists to better understand which factors influence physician’s treatment choice.
Objective
The ongoing prospective phase 2 TAILOR study assesses the efficacy and safety of FD I+V and continuous ibrutinib monotherapy using proactively reduced dose design and reactive dose adjustment per label in patients with previously untreated CLL (NCT05963074). A questionnaire was designed to capture the decision-making factors influencing either FD I+V or continuous ibrutinib monotherapy.
Methods
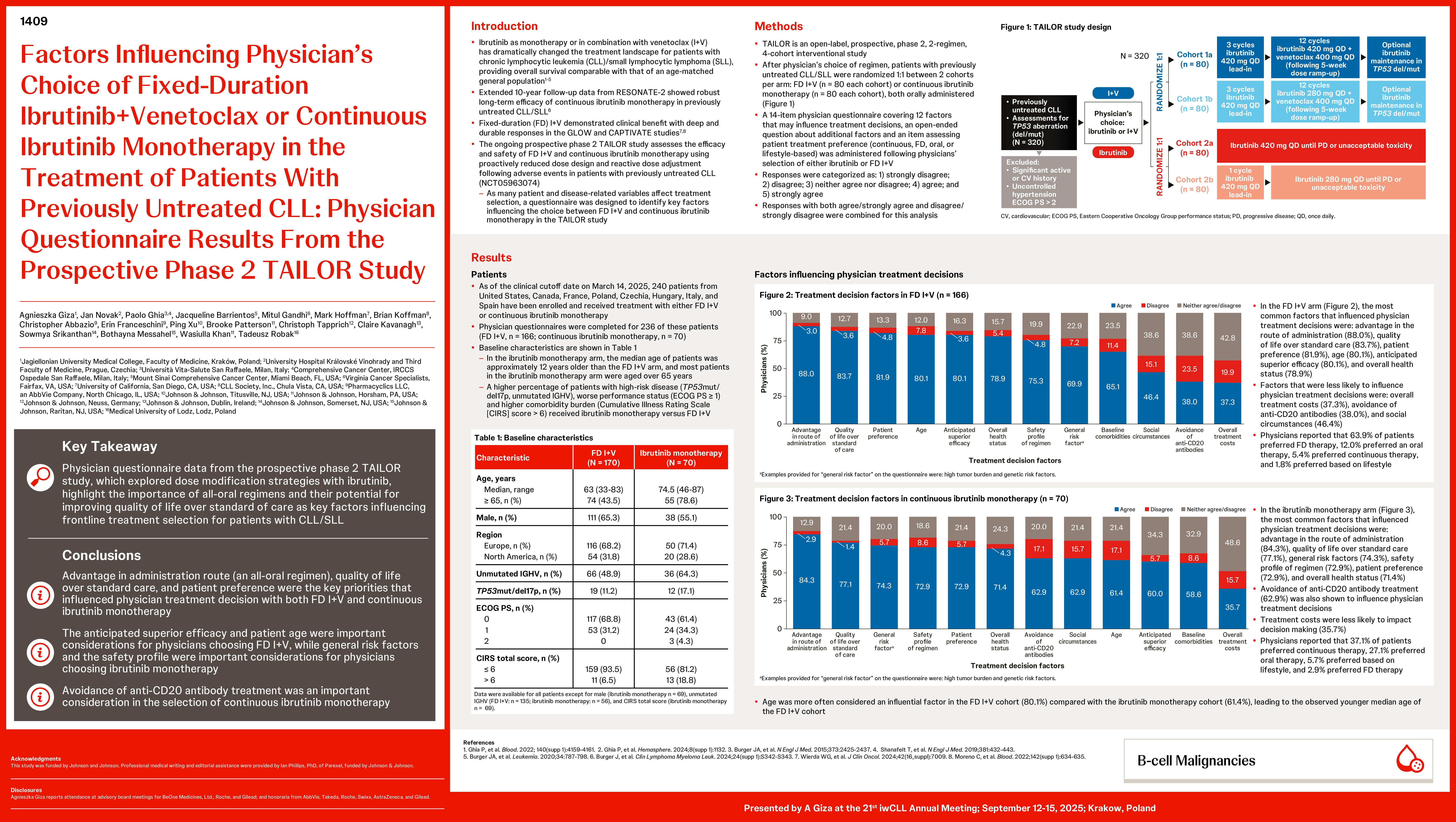
TAILOR is an open-label, prospective, phase 2, 2-regimen, 4-cohort interventional study. After physician’s choice of regimen, patients with previously untreated CLL/SLL were randomized 1:1 between 2 cohorts per arm: FD I+V (n=80 each cohort) or continuous ibrutinib monotherapy (n=80 each cohort).
A physician questionnaire was used to determine factors that influence treatment decisions. These parameters were age, general risk factors, baseline comorbidities, anticipated superior efficacy, avoidance of anti-CD20 antibodies, advantage in route of administration, overall health status, overall treatment costs, safety profile of regimen, social circumstances, patient preference, and quality of life. Responses were categorized as: 1) strongly disagree; 2) disagree; 3) neither agree nor disagree; 4) agree; and 5) strongly agree. Responses with both agree/strongly agree and disagree/strongly disagree were combined for this analysis.
Results
As of the clinical cutoff date on March 14, 2025, 240 patients from United States, Canada, France, Poland, Czechia, Hungary, Italy, and Spain have been enrolled and received treatment with either FD I+V or continuous ibrutinib monotherapy, and physician questionnaires were completed for 236 of these patients (FD I+V, n=166; continuous ibrutinib monotherapy, n=70). As of April 10, 2025, 63 of 64 investigators who have screened or enrolled patients have completed the physician treatment questionnaire.
Among patients who received FD I+V, 43.5% were aged ≥65 years, 65.3% were male, 68.2% were from Europe and 31.8% from North America, 11.2% had TP53/del17p mutations, and 48.9% had unmutated immunoglobulin heavy chain variable (uIGHV) genes. The 5 most common factors that influenced physician treatment decisions included advantage in the route of administration (88.0%), quality of life over standard care (83.7%), patient preference (81.9%), age (80.1%), and anticipated superior efficacy (80.1%). Factors that were less likely to influence physician treatment decisions included overall treatment costs (37.3%), avoidance of anti-CD20 antibodies (38.0%), and social circumstances (46.4%). When asked, 63.9% of physicians preferred FD I+V.
Among patients who received continuous ibrutinib monotherapy, 78.6% were aged ≥65 years, 55.1% were male, 71.4% were from Europe and 28.6% from North America, 17.1% had TP53/del17p mutations, and 64.3% had uIGHV. The 5 most common factors that influenced physician treatment decisions included advantage in the route of administration (84.3%), quality of life over standard care (77.1%), general risk factors (74.3%), safety of regimen (72.9%), and patient preference (72.9%). Avoidance of anti-CD20 antibody treatment (62.9%) was also shown to influence physician treatment decisions, while treatment costs were less likely to impact decision making (35.7%).
Conclusions
Data from this prospective study provide important perspectives from physicians regarding the choice of FD I+V or continuous ibrutinib monotherapy in the first-line treatment of patients with CLL. These data show that advantage in administration route (an all-oral regimen), quality of life over standard care, and patient preference were the key priorities that influenced physician treatment decision with both FD I+V and continuous ibrutinib monotherapy. Avoidance of anti-CD20 antibody treatment was an important consideration in the selection of continuous ibrutinib monotherapy but less so for FD I+V. These results can help further inform and facilitate improved shared decision-making approaches between physicians and patients when selecting a frontline treatment option to treat CLL/SLL.
Keywords : ibrutinib-venetoclax (TAILOR), physician-questionnaire, treatment-decision
Please indicate how this research was funded. : This study was funded by Johnson and Johnson
Please indicate the name of the funding organization.: Johnson and Johnson