Authors
Constantine S. Tam, MBBS, MD, Paul M. Barr, MD, John N. Allan, MD, Tanya Siddiqi, MD, Alessandra Tedeschi, MD, Thomas J. Kipps, MD, PhD, Susan M. O’Brien, MD, Ryan Jacobs, MD, Xavier C. Badoux, MBBS, FRACP, FRCPA, Livio Trentin, MD, Masa Lasica, MBBS, FRACP, FRCPA, Dennis Carney, MBBS, FRACP, FRCPA, Anna Elinder Camburn, MBChB, FRACP, FRCPA, Javier De la Serna, MD, Edith Szafer-Glusman, PhD, Cathy Zhou, MS, Jutta K. Neuenburg, MD, PhD, James P. Dean, MD, PhD, Paolo Ghia, MD, PhD, William G. Wierda, MD, PhD.
Background
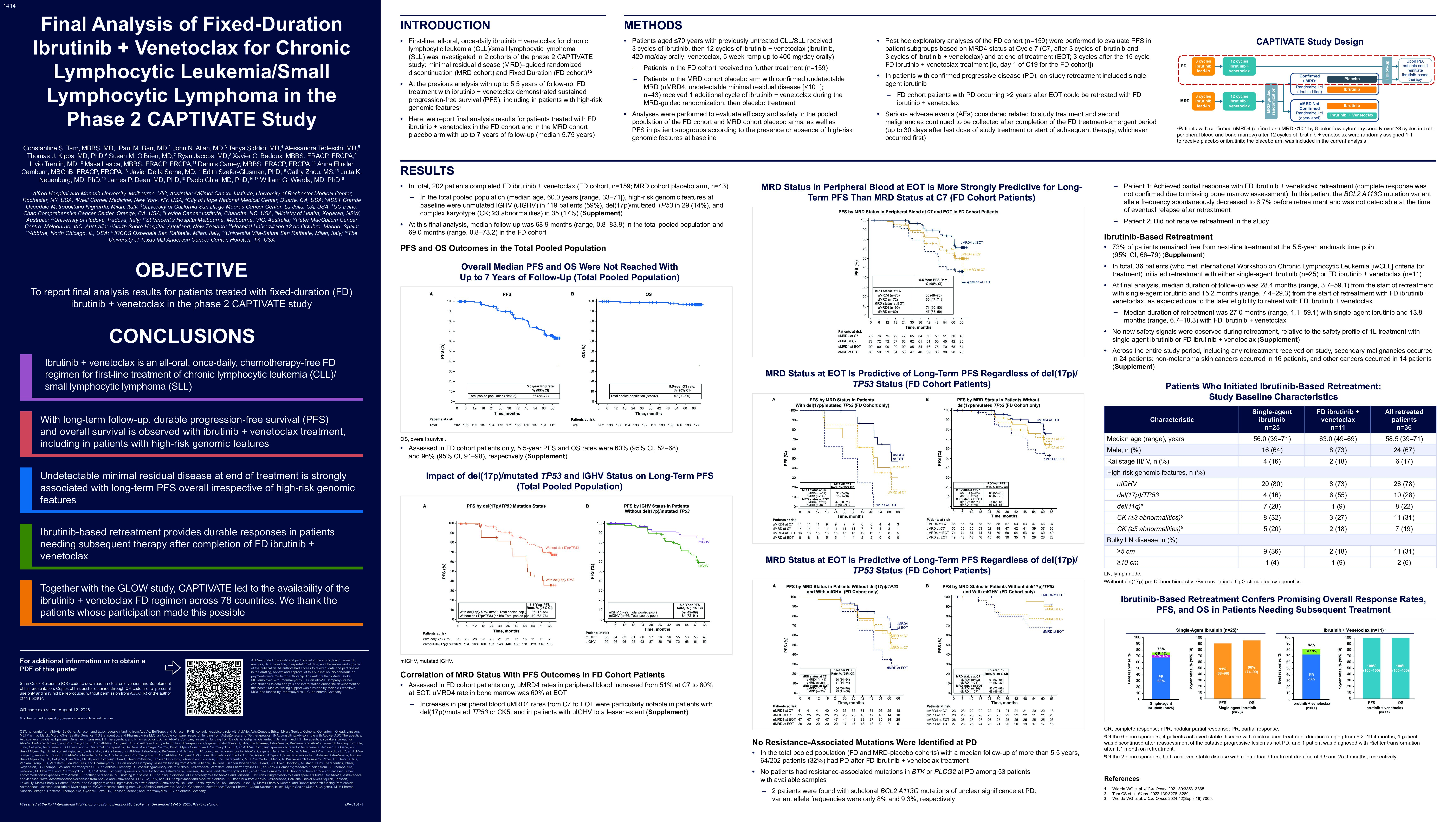
First-line ibrutinib (Ibr) + venetoclax (Ven) treatment for chronic lymphocytic leukemia/ small lymphocytic lymphoma (CLL/SLL) was tested in the phase 2 CAPTIVATE study, including minimal residual disease (MRD)–guided randomized discontinuation (MRD cohort) and Fixed Duration (FD) cohorts. We report final analysis results for patients treated with FD Ibr+Ven in the FD cohort and MRD cohort placebo arm.
Methods
Patients aged ≤70 years with previously untreated CLL/SLL received 3 cycles of Ibr, then 12 cycles of Ibr+Ven (Ibr, 420 mg/day orally; Ven, 5-week ramp up to 400 mg/day orally), up to 13 cycles in the MRD cohort placebo arm. On-study retreatment included single-agent Ibr; FD cohort patients with progressive disease (PD) >2 years after end of treatment (EOT) could be retreated with FD Ibr+Ven.
Results
A total of 202 patients completed FD Ibr+Ven (FD cohort, n=159; MRD cohort placebo arm, n=43). With a median follow-up of 68.9 months (range, 0.8–83.9), 5.5-year progression-free survival (PFS) and overall survival (OS) rates (95% CI) were 66% (58–72) and 97% (93–99), respectively. 5.5-year PFS rates (95% CI) in patients without and with del(17p)/mutated TP53 were 70% (62–76) and 36% (17–55), respectively. In patients with unmutated IGHV, 5.5-year PFS was 55% (45–64): 63% (49–74) in patients without, and 44% (28–60) in patients with, concomitant del(17p)/mutated TP53/complex karyotype. The corresponding rates for patients with mutated IGHV were 79% (68–87), 85% (71–93), and 62% (34–81). Undetectable MRD (uMRD4; < 10–4 by flow cytometry) was achieved in peripheral blood (PB) in 54% of patients at C7 and 69% at EOT, and in bone marrow in 69% of patients at EOT. 5.5-year PFS rates (95% CI) were higher in patients with uMRD4 in PB at EOT (75% [67–82]) vs those with MRD (47% [33–59]). 64 patients had PD after completion of FD Ibr+Ven. 5.5-year freedom from next-line treatment was 73% (95% CI 66–79). Of 40 patients with available samples at PD to date, 1 had an acquired subclonal mutation in BCL2 of unclear significance (A113G, VAF 8.3%); none had acquired resistance-associated mutations in BTK or PLCG2. 36 patients initiated retreatment with Ibr (n=25) or Ibr+Ven (n=11). With 28.4 months median follow-up on Ibr retreatment (range, 3.7–59.1), overall response rate (ORR) was 76% (best response: 1 complete response [CR]; 1 nodular partial response [PR]; 17 PR; 4 stable disease [SD]; 1 PD [Richter transformation]; 1 no assessment); 2-year PFS and OS rates from the start of retreatment were 91% and 96%, respectively. With 15.2 months median follow-up on Ibr+Ven retreatment (range, 7.4–29.3), ORR was 82% (best response: 1 CR; 8 PR; 2 SD); 1-year PFS and OS rates from the start of retreatment were both 100%. Second malignancies occurred in 24 patients across the entire study period, including 12 initial treatment and 4 retreatment treatment emergent adverse events.
Conclusions
Ibr+Ven is an all-oral, once-daily, chemotherapy-free FD regimen for first-line treatment of CLL/SLL that continues to provide durable PFS and OS with long-term follow-up, including in patients with high-risk genomic features. Ibr-based retreatment provided durable responses in patients needing subsequent therapy after completion of FD Ibr+Ven.
Keywords : CLL/SLL, ibrutinib+venetoclax, fixed-duration treatment
Please indicate how this research was funded.: Funded by Pharmacyclics
Please indicate the name of the funding organization. : Funded by Pharmacyclics