Authors
David Allsup, David A Cairns, Faye Samy, Lelia Duley, Adrian Bloor, David Meads, Bryony Dawkins, Sean Girvan, Dena Howard, Julia Brown, Anna Hockaday, Sue Bell, Sharon Jackson, Natasha Greatorex, Surita Dalal, Piers Patten, Peter Hillmen, Talha Munir.
Background
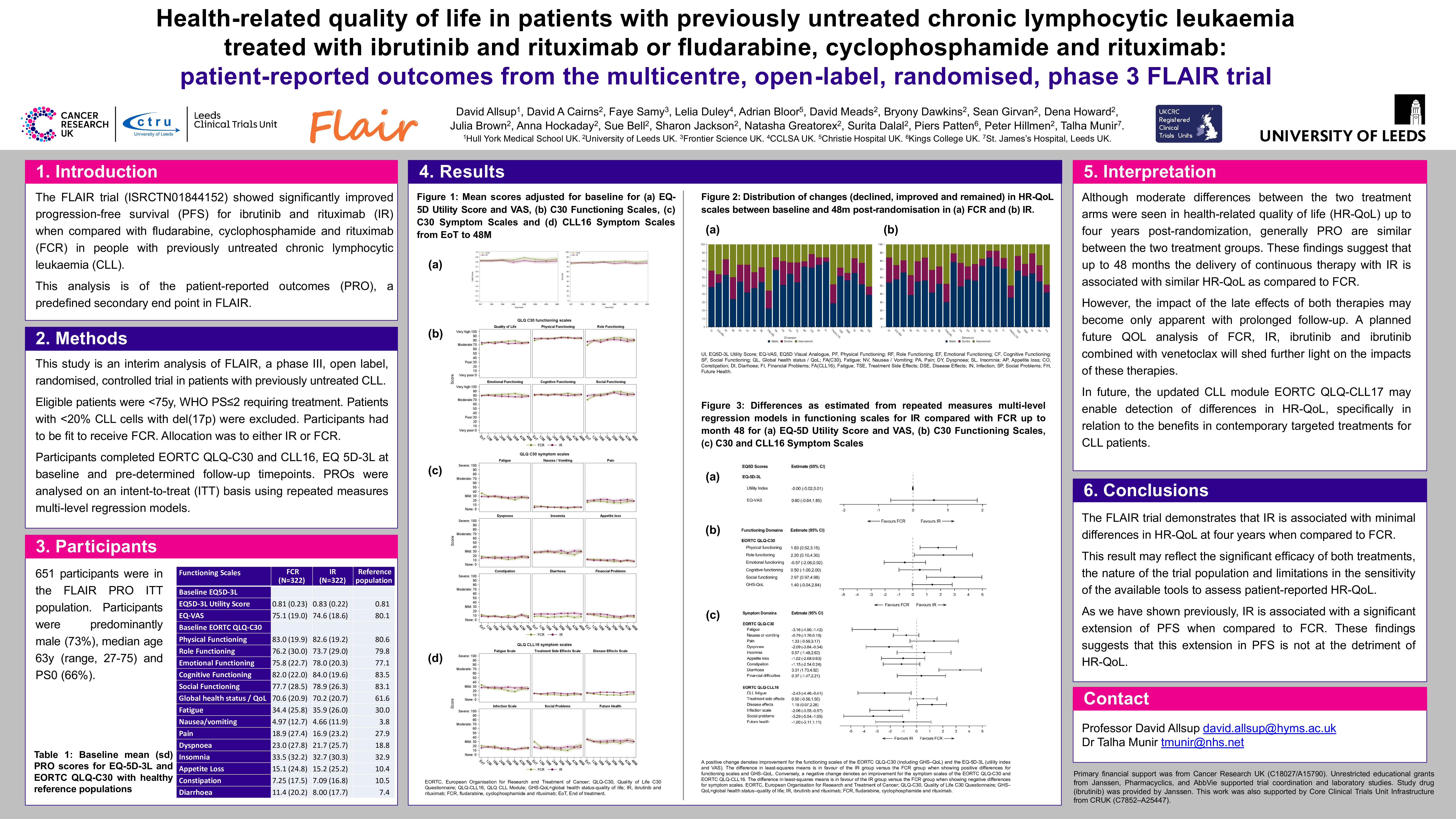
The FLAIR trial showed significantly improved progression-free survival (PFS) for ibrutinib and rituximab (IR) when compared with fludarabine, cyclophosphamide and rituximab (FCR) in people with previously untreated chronic lymphocytic leukaemia (CLL). This analysis is of the patient-reported outcomes (PROs), a predefined secondary end point in FLAIR.
Methods
This study is an interim analysis of FLAIR, a phase three, open label, randomised, controlled trial in persons with previously untreated CLL conducted at 101 UK National Health Service (NHS) hospitals. Eligible patients were between 18 and 75 years of age with a World Health Organisation (WHO) performance status (PS) of two or less and disease status requiring treatment according to iwCLL criteria. Those with more than 20% of CLL cells with d17p were excluded. Participants had to be fit to receive FCR and have adequate renal function. Participants were randomly assigned (1:1) using minimisation with a random element in a web-based system. Stratification was by Binet stage, age, sex, and centre. Allocation was to either IR (ibrutinib 420mg/day orally for 6 years, until minimal residual disease stopping rules were reached, until toxicity requiring cessation or until disease progression, whichever occurred first with rituximab: 375/500 mg/m2 IV on day 1 of cycle 1/2-6 of a 28-day cycle) or FCR (fludarabine 24 mg/m2/day orally on day 1-5, cyclophosphamide 150 mg/m2/day orally on day 1-5 and rituximab: as for FCR). The primary end point was PFS.
Participants completed the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life C30 Questionnaire (QLQ-C30), Chronic Lymphocytic Leukaemia Module (QLQ-CLL16), Euroqol 5 dimensions (EQ-5D-3L), and EQ-5D visual analogue scale (VAS) at baseline and pre-determined follow-up timepoints. PROs included function and symptom scales which were analysed on an intention to treat basis using repeated measures multi-level regression models.
FLAIR is ISRCTN and clinicaltrialsregister.eu registered (ISRCTN01844152 and 2013-001944-76).
Findings
651 of 771 (84.4%) FLAIR participants completed the baseline PROs. Compliance was good up to 48 months. Characteristics of the PRO population were similar to all FLAIR participants. Median age was 63 years, 27% were female and the majority identified their ethnicity as white. Observed trajectories in quality of life (QOL) were similar between participants treated with IR and FCR for the EQ-5D, EORTC-QLQ-C30 and EORTC-QLQ-CLL16. Several scales showed worse function or symptoms at the end of FCR treatment, but such scores recovered to ultimately be equivalent, or better than those for IR at 48 months.
A comparison between baseline and 48-month timepoints showed that higher proportions of FCR-treated participants experienced improvement for the EQ-Utility Index, EQ-VAS, cognitive functioning, fatigue, diarrhoea, treatment side effects, disease effects and infections scales.
The estimated mean differences from repeated measures multi-level modelling were not statistically significant for the EQ-5D Utility Score or EQ-VAS. Physical functioning, role functioning and social functioning were statistically significant in favour of IR. In contrast emotional function measures favoured FCR. Symptoms of diarrhoea were lower in the FCR group, whilst fatigue and dyspnoea were higher. Disease effects were lower in those allocated FCR, but CLL-related fatigue, infection and social problems were lower in those allocated IR. The observed differences in all symptom scales did not exceed the between-group minimally important difference for improvement.
Interpretation
Although moderate differences between the two treatment arms were seen in HR-QoL up to four years post-randomization, generally PROs are similar between the two treatment groups. These findings suggest that up to 48 months the delivery of continuous therapy with IR is associated with similar HR-QoL as compared to FCR. However, the impact of the late effects of both therapies may become only apparent with prolonged follow-up. A planned future QOL analysis of FCR, IR, ibrutinib and ibrutinib combined with venetoclax will shed further light on the impacts of these therapies. In future, the updated CLL module EORTC QLQ-CLL17 may enable detection of differences in HR-QoL, specifically in relation to the benefits in contemporary targeted treatments for CLL patients.
Keywords : leukaemia, therapy, quality of life
Please indicate how this research was funded. : Primary financial support was from Cancer Research UK [ C18027/A15790 ]. Unrestricted educational grants from Janssen, Pharmacyclics and AbbVie supported trial coordination and laboratory studies. Study drug (ibrutinib) was provided by Janssen. This work was also supported by Core Clinical Trials Unit Infrastructure from CRUK [ C7852/A25447 ].
Please indicate the name of the funding organization.: Cancer Reseach UK
Johnson and Johnson