Authors
S. Molica, P.R. Scalzulli, L. Scarfò, C. Minoia, R. Murru, P. Sportoletti, F. Frigeri, F. Albano, N. Di Renzo, A. Sanna, L. Laurenti, M. Massaia, R. Cassin, M. Coscia, C. Patti, E. Pennese16, A. Tafuri, A. Chiarenza, P. Galieni, O. Perbellini, C. Selleri, C. Califano, F. Ferrara, A. Cuneo, M. Murineddu, G. Palumbo, I. Scortechini, A. Tedeschi, L. Trentin, M. Varettoni, F. Pane31, F. Merli, L. Morello, G. Musuraca, M. Tani, A. Ibatici, M. Palma, F.R. Mauro.
Background
Despite the introduction of second-generation BTK inhibitors (BTKis), ibrutinib remains central to chronic lymphocytic leukemia (CLL) management. However, dose reductions due to adverse events may compromise efficacy, underscoring the importance of sustained adherence.
Aim
This study investigates factors associated with ibrutinib dose reduction and assesses the impact of adherence to the full prescribed dose on progression-free (PFS) and overall survival (OS) in patients with CLL treated in routine clinical practice. Particular focus is given to adherence during the first 90 days, a period critical to long-term outcomes.
Methods
We analyzed data from the EVIdeNCE study (NCT03720561), a multicenter, observational, prospective, cohort study conducted at 39 hematological institutions in Italy between November 2018 and October 2019. The study enrolled consecutive adult patients with a confirmed diagnosis of CLL who started treatment with ibrutinib in either first-line or more advanced line as part of routine clinical practice.
Adherence was calculated for each patient, as the ratio between the average daily dose received during the specified timeframe (i.e., total cumulative dose divided by the number of days) and the full prescribed daily dose of 420 mg.
A 100% adherence to treatment indicates that patients received the full daily dose throughout the evaluated period. Treatment interruptions or discontinuations were accounted for by assigning a dose of 0 mg per day for the corresponding days.
For the purpose of the analysis, ibrutinib adherence was assessed at 30, 60, and 90 days of treatment.
Finally, we analyzed the associations between adherence and clinical outcomes (PFS and OS) using both unadjusted and multivariable models. Models were adjusted for patient and disease characteristics.
Results
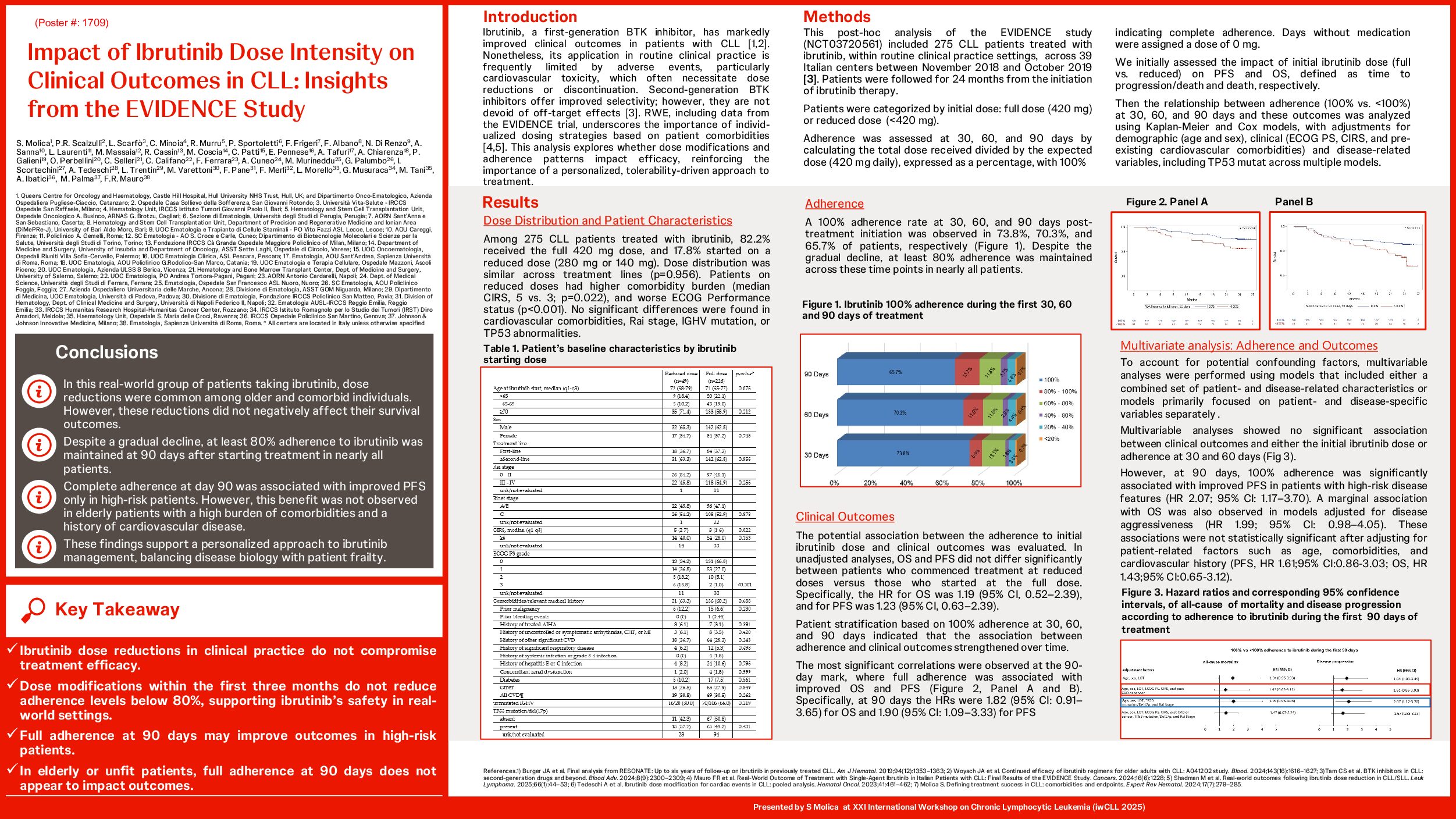
Data from 275 CLL patients receiving ibrutinib either as a first-line (37%) or subsequent line (67%) treatment were analyzed. Among them, 82.2% received the full dose of ibrutinib (420 mg), while 17.8% required dose reductions (26 patients at 280 mg and 23 at 140 mg). Dose adjustments were equally distributed among patients who received ibrutinib as first or subsequent line of therapy (p=0.956).
Patients in the reduced-dose cohort exhibited significantly higher median CIRS scores (5 vs. 3, p = 0.022) and poorer ECOG PS (p < 0.001) compared to those who maintained the full dose. While age differences approached significance (p = 0.076), no significant differences were observed in CIRS subdomains or specific comorbidities, including cardiovascular diseases (p = 0.262).
Adherence to the full prescribed dose declined over time—73.8% at 30 days, 70.3% at 60 days, and 65.7% at 90 days—yet approximately 80% of patients maintained ≥80% adherence throughout.
In the unadjusted analyses, initial dose reduction did not significantly affect OS (HR: 1.19, 95% CI: 0.52–2.39) or PFS (HR: 1.23, 95% CI: 0.63–2.39). In contrast, maintaining full treatment adherence (100%) at 90 days was significantly associated with improved PFS (HR: 1.90, 95% CI: 1.09–3.33), particularly among patients with high-risk disease features (TP53 mutations or deletion 17p, advanced Rai stage; PFS: HR 2.07, 95% CI: 1.17–3.70).
However, this association was no longer observed after adjusting for patient-related factors, including advanced age and high comorbidity burden (OS: HR 1.47, 95% CI: 0.67–3.24; PFS: HR 1.23, 95% CI: 0.65–2.31).
Conclusions
In this analysis of the EVIDENCE trial, maintaining 100% adherence to the prescribed ibrutinib dose at 90 days was significantly associated with improved PFS in patients with high-risk CLL. Conversely, among elderly or unfit patients, an adherence rate of at least 80% appeared sufficient to achieve comparable clinical outcomes. These findings underscore the importance of individualized adherence strategies—highlighting the critical role of strict adherence in high-risk patients, while lower adherence thresholds may remain appropriate for select patient subgroups.
Keywords : Chronic lymphocytic leukemia, ibrutinib
Please indicate how this research was funded. : Company sponsored study
Please indicate the name of the funding organization.: Johnson&Johnson Innovative Medicine, Italy