Authors
Brian Koffman, Xiaoliang Wang, Qianhong Fu, Dong Yuan, Derrick van Beuge, Gregory A. Maglinte, Erlene K. Seymour.
Background
Genetic markers like del17p, TP53 mutation (TP53m), and immunoglobulin heavy variable chain mutation (IGHVm) are important for chronic lymphocytic leukemia (CLL) prognosis. Del17p, TP53m, and unmutated IGHV are associated with early disease progression, particularly among patients receiving chemoimmunotherapy (CIT) and ibrutinib. Knowledge is limited on the impact of genetic testing on front-line (1L) treatment choices and clinical outcomes in CLL.
Methods
This retrospective cohort study utilized the US electronic health record-derived de-identified Flatiron Health Research Database. Eligible patients included adults with CLL diagnosis who started 1L treatment 01/01/2020-30/11/2024. Primary exposures included evidence of testing any time before 1L initiation, regardless of testing status. Tests included FISH for del17p, DNA sequencing for TP53m, and IGHV. Descriptive statistics were summarized by each test and by combining patients with del17p and TP53m. Primary exposures consisted of combined del17p/TP53 and IGHV tests, including patients who received tests before 1L as the reference group. Outcomes included real-world time to next treatment or death (rwTTNT) and OS (rwOS) from 1L initiation. Landmark treatment and survival probabilities were estimated using Kaplan-Meier method. HRs and 95% CIs were estimated using Cox proportional hazard models, adjusting for age, sex, race/ethnicity, insurance, comorbidity, socioeconomic status, practice type, Rai stage, year of 1L initiation, and Eastern Cooperative Oncology Group (ECOG) performance status (PS). Stratified analyses were performed by 1L treatment, including CIT, ibrutinib, and National Comprehensive Cancer Network® (NCCN) guideline–preferred novel therapies (NTs; acalabrutinib, zanubrutinib, venetoclax-based therapies). In exploratory analyses, the proportion of patients with 1L treatment by testing result was summarized.
Results
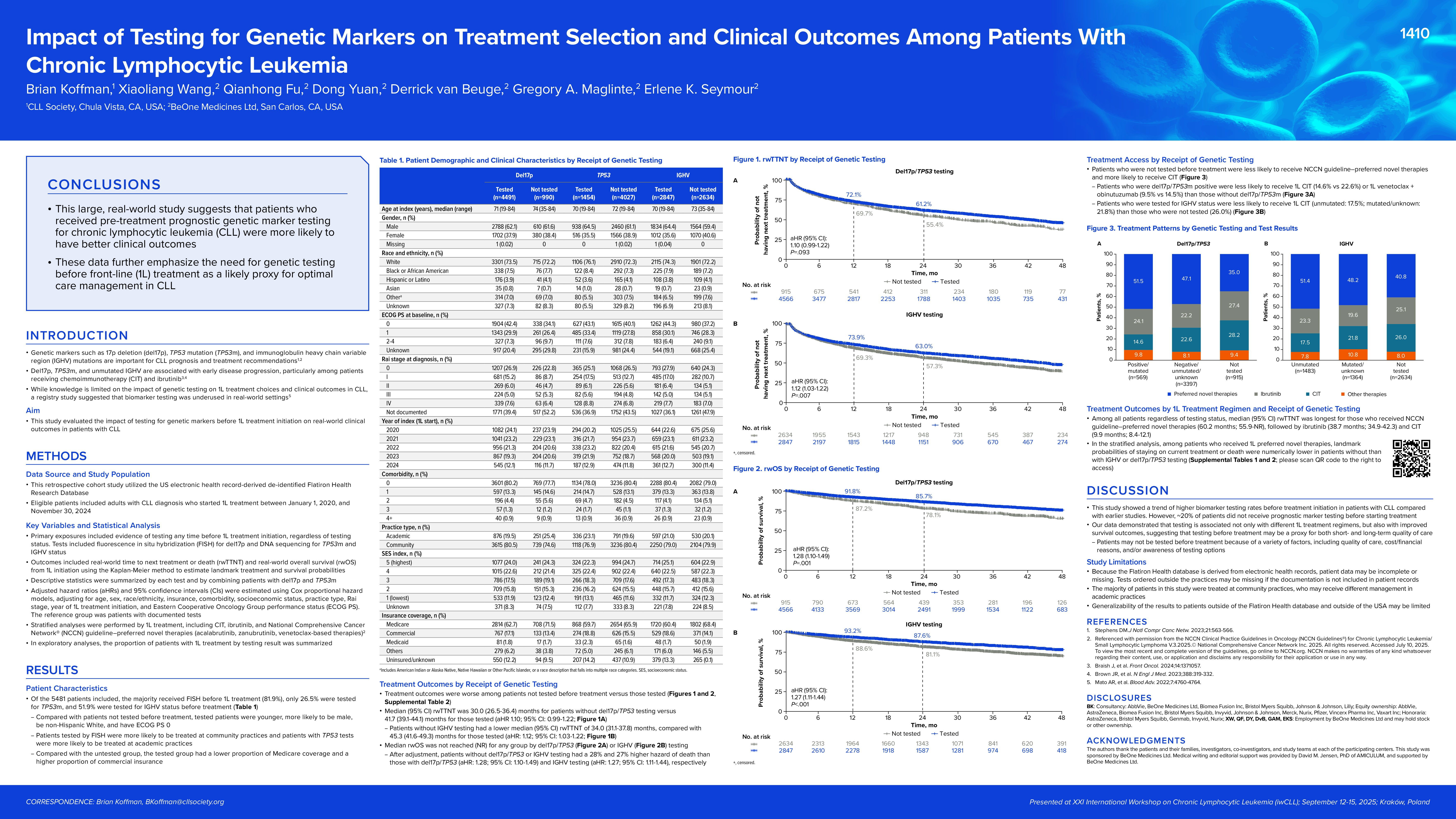
Of the 5481 patients included, the majority received FISH before 1L treatment (81.9%) and only 26.5% were tested for TP53m. About half of patients were tested for IGHV before treatment (51.9%). Compared with patients not tested before treatment, tested patients were younger (median age: 71 vs 75 [del17p/TP53], 70 vs 73 [IGHV]), more likely to be male (65% vs 61% [TP53], 64% vs 59% [IGHV]), non-Hispanic White (74% vs 72% [del17p/TP53 and IGHV]), and had ECOG PS 0 (42% vs 33% [del17p/TP53], 44% vs 37% [IGHV]). Patients tested by FISH were more likely to be treated at community practices (80% vs 75%) and patients with TP53 tests were more likely to be treated at academic practices (23% vs 20%). Patients tested for IGHV status were more likely to have commercial insurance (31% vs 26%) and less likely to have Medicare (45% vs 50%).
Survival outcomes were worse among patients not tested before treatment versus those tested. Median rwTTNT was 30.0 months for patients without del17p/TP53 testing (95% CI 26.5-36.4) versus 41.7 months (95% CI 39.1-44.1) for those tested (HR 1.10; 95% CI 0.99-1.23). Patients without IGHV testing had lower median rwTTNT of 34.0 months (95% CI 31.1-37.8) than 45.3 months (95% CI 41.6-49.3) for those tested (adjusted HR 1.12; 95% CI 1.03-1.22). Median rwOS was not reached (NR) for any group. After adjustment, patients without IGHV or del17p/TP53 testing had 27% and 26% higher hazards of death than those with IGHV testing (HR 1.27; 95% CI 1.12-1.44) and del17p/TP53 testing (HR 1.26; 95% CI 1.09-1.47), respectively.
Additionally, patients who were not tested before treatment were less likely to receive NCCN guideline–preferred NTs (del17p/TP53: 35% vs 48%; IGHV: 41% vs 50%) and more likely to receive CIT (del17p/TP53: 28% vs 22%; IGHV: 26% vs 20%). Further stratified by test results, patients who were del17p/TP53m-positive were less likely to receive 1L CIT (15% vs 23%) or 1L venetoclax+obinutuzumab (9% vs 14%) than those without del17p/TP53m. Among all patients, median (95% CI) rwTTNT was longest for those who received NCCN guideline–preferred NTs (60.2 months; 55.9-NR), followed by ibrutinib (38.7 months; 34.9-42.3) and CIT (9.9 months; 8.4-12.1). In the stratified analysis, among patients who received 1L NTs, landmark probabilities of staying on current treatment or death were numerically lower in patients without than with IGHV testing (12 months: 82% vs 85%; 24 months: 71% vs 76%) or del17p/TP53 testing (81% vs 84%; 70% vs 74%).
Conclusion
This large, real-world study suggests patients who received pre-treatment prognostic genetic marker testing for CLL were more likely to have better clinical outcomes, further emphasizing the need for testing before 1L treatment as a likely proxy for optimal care management in CLL.
Keywords : Biomarker testing
Treatment patterns
Survival outcomes
Please indicate how this research was funded. : This study is funded by BeOne Medicines Ltd.
Please indicate the name of the funding organization.: BeOne Medicines Ltd.