Incidence of second primary malignancies in Chronic lymphocytic leukemia (878kB pdf)
Authors
Regina Zsigmond, Előd János Zsigmond, Zita Borbényi, Adrienn Sulák, Blanka Godza, Tímea Gurbity Pálfi.
Introduction
Chronic lymphocytic leukemia (CLL) involves a broad spectrum of genetic mutations and is treated with multiple therapeutic approaches. This disorder may be associated with second primary malignancies (SPM), including solid tumors (ST) and other hematologic neoplasms (HN), potentially due to therapy side effect and genetic predisposition.
Aim
This study aimed to evaluate the incidence and and long-term prognostic value of SPM in CLL patients.
Method
We conducted a retrospective analysis at the Hematology Department of the University of Szeged including consecutive CLL patients from January 2012 to January 2025. The study assessed the prevalence of SPM, the influence of therapy and genetic background on SPM development, and the long-term prognostic significance of SPM.
Results
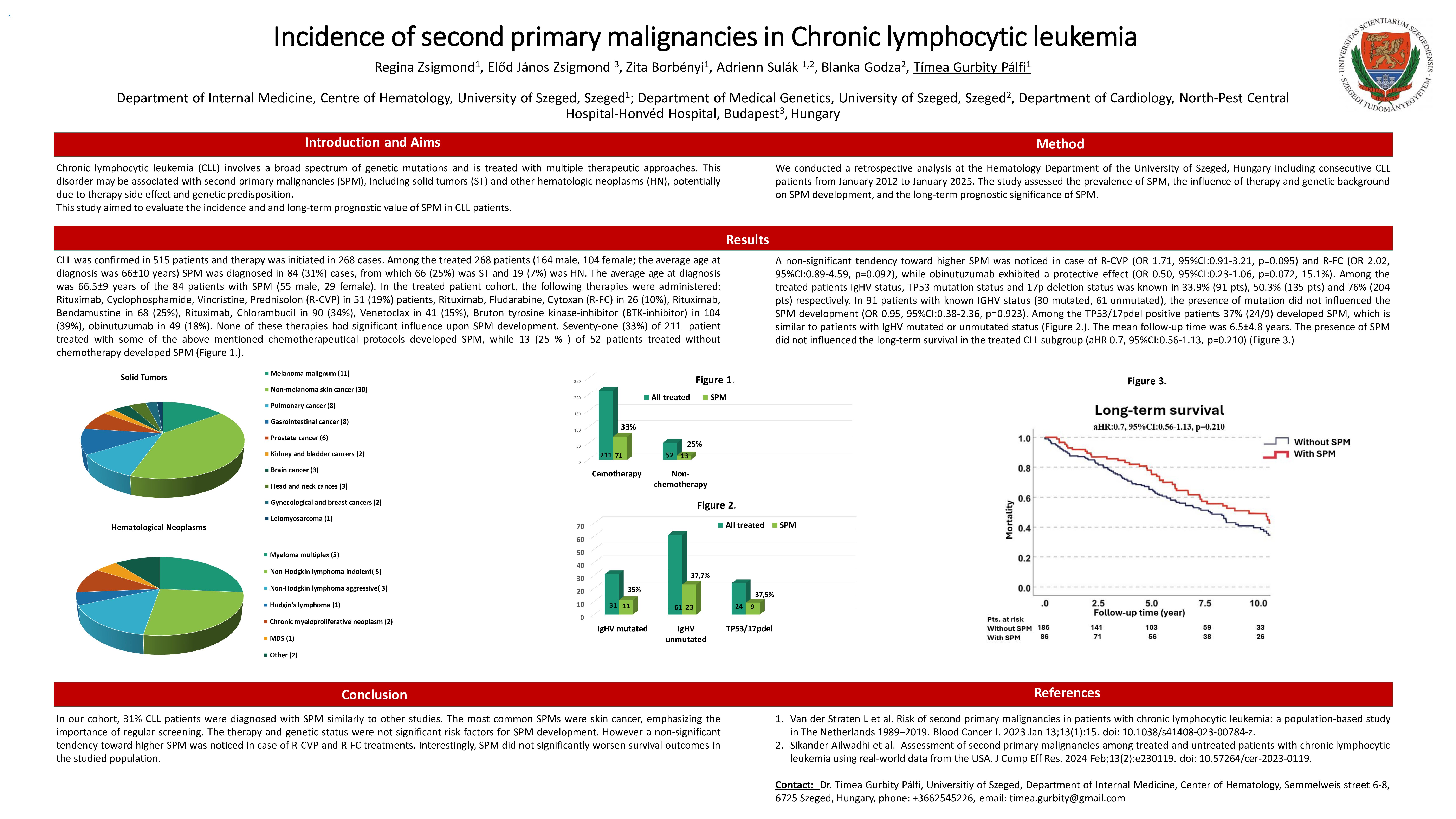
CLL was confirmed in 515 patients and therapy was initiated in 268 cases. Among the treated 268 patients (164 male, the average age at diagnosis was 66±10 years) SPM was diagnosed in 84 (31%) cases, from which 66 (25%) was ST and 19 (7%) was HN.
In the treated patient cohort the following therapies was administreted: Rituximab, Cyclophosphamide, Vincristine, Prednisolon (R-CVP) in 51 (19%) patients, Rituximab, Fludarabine, Cytoxan (R-FC) in 26 (10%), Rituximab, Bendamustine in 68 (25%), Rituximab, Chlorambucil in 90 (34%), Venetoclax in 41 (15%), Bruton tyrosine kinase-inhibitor (BTK-inhibitor) in 104 (39%), obinutuzumab in 49 (18%). Non of these therapies had significant influence upon SPM developement. A non-significant tendency toward higher SPM was noticed in case of R-CVP (OR 1.71, 95%CI:0.91-3.21, p=0.095) and R-FC (OR 2.02, 95%CI:0.89-4.59, p=0.092), while obinutuzumab exhibited a protective effect (OR 0.50, 95%CI:0.23-1.06, p=0.072, 15.1%). In 91 patients with known IGHV status (30 positive, 61 negative) the presence of mutation did not influenced the SPM developement (OR 0.95, 95%CI:0.38-2.36, p=0.923). Further genetic results are still in progress. The mean follow-up time was 6.5±4.8 years. The presence of SPM did not influenced the long-term survival in the treated CLL subgroup (aHR 0.7, 95%CI:0.56-1.13, p=0.210).
Conclusion
In our cohort, 31% CLL patients were diagnosed with SPM, emphasizing the importance of regular screening. The therapy and genetic status were not significant risk factors for SPM development. Interestingly, SPM did not significantly worsen survival outcomes in the studied population.
Keywords : Cll, SPM, incidence
Please indicate how this research was funded. : It is the work of a hematology resident doctor, not financially funded.
Please indicate the name of the funding organization.: It has been supported, by the Hematology Department, University of Szeged, Hungary