Authors
Mazyar Shadman, David Campbell, Mei Xue, Marjan Massoudi, Keri Yang, Rhys Williams, Asher Chanan-Khan.
Introduction
Bruton tyrosine kinase inhibitors (BTKis), including zanubrutinib and acalabrutinib, have become a standard of care in chronic lymphocytic leukemia (CLL). However, there is a lack of head-to-head comparative trial data. In the phase 3 ALPINE study (NCT03734016), zanubrutinib showed favorable progression free survival (PFS) compared to ibrutinib in the treatment of relapsed/refractory (R/R) CLL. In the ASCEND study (NCT02970318), acalabrutinib showed improved PFS vs rituximab-idelalisib/bendamustine in R/R CLL. A previously published matching-adjusted indirect comparison (MAIC) reported significantly improved PFS and complete response rates for zanubrutinib compared to acalabrutinib (Shadman 2024). This study aimed to compare zanubrutinib versus acalabrutinib in R/R CLL by calculating the number needed to treat (NNT) to avoid one progression or death and associated incremental costs.
Methods
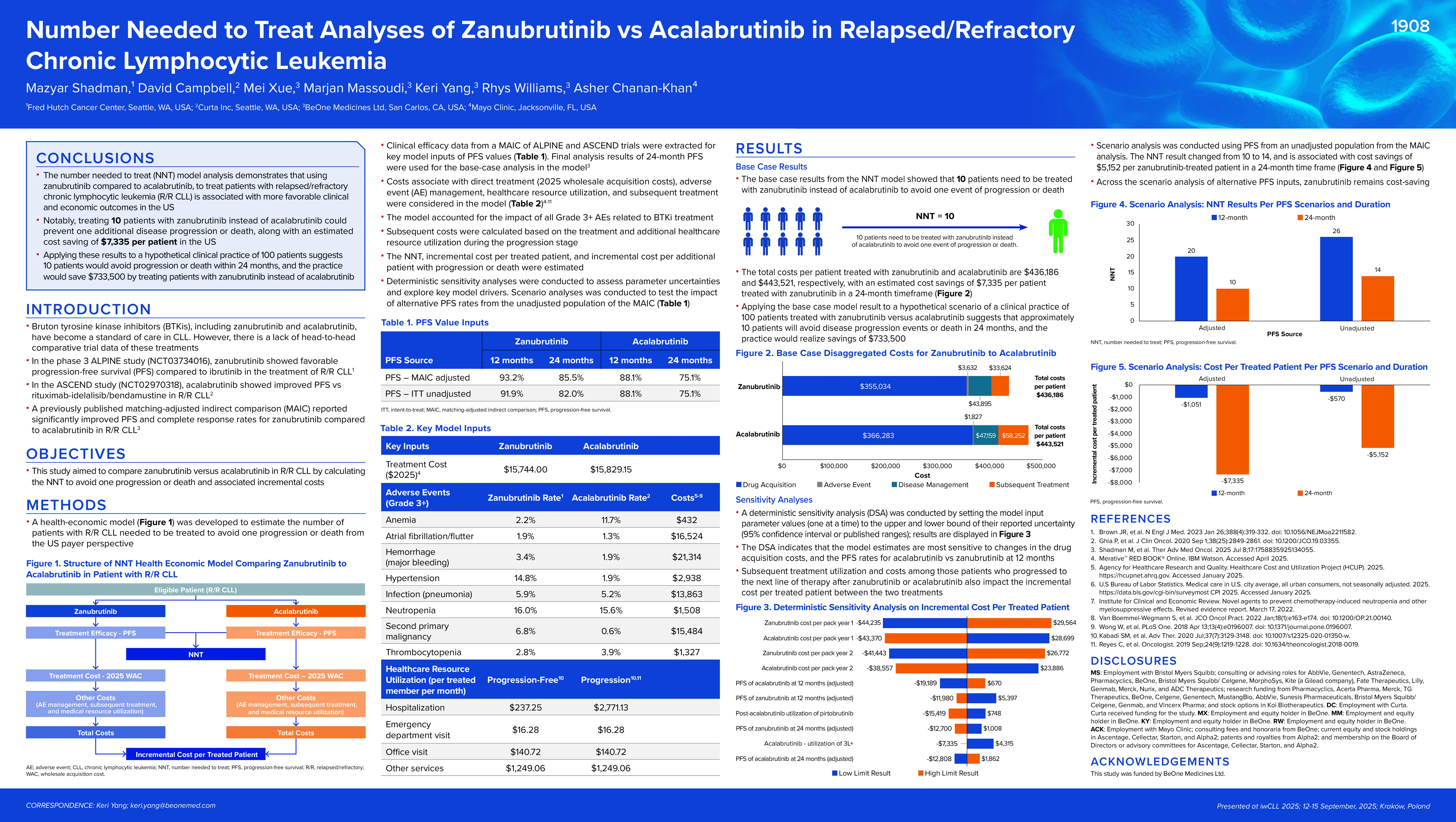
A health-economic model was developed to estimate the number of R/R CLL patients needed to be treated to avoid one progression or death from the US payer perspective. Clinical efficacy data from a MAIC of ALPINE and ASCEND trials were extracted. Final analysis results of 24-month PFS (85.5% for zanubrutinib and 75.1% for acalabrutinib) were used for the base-case analysis in the model. Costs associate with direct treatment (2025 wholesale acquisition costs), adverse event management, healthcare resource utilization, and subsequent treatment were considered in the model. The NNT, incremental cost per treated patient, and incremental cost per additional patient with progression or death were estimated. Deterministic sensitivity analyses were conducted to assess parameter uncertainties and explore key model drivers. Sensitivity analyses were conducted to test the impact of alternative PFS rates from the unadjusted population of the MAIC.
Results
The base-case results from the NNT model showed that for every 10 patients treated with zanubrutinib instead of acalabrutinib, one event of progression or death would be avoided. The total costs per patient treated with zanubrutinib and acalabrutinib are $436,186 and $443,521, respectively, with a cost savings of $7,335 associated with using zanubrutinib in a 24-month timeframe. Drug costs and PFS have the greatest impact on the incremental cost per patient. A sensitivity analysis was conducted using PFS from an unadjusted population from the MAIC analysis. The NNT result changed from 10 to 14 and is associated with cost savings of $5,152 per zanubrutinib-treated patient in a 24-month time frame. Applying the base-case model result to a hypothetical scenario of a clinical practice of 100 patients treated with zanubrutinib versus acalabrutinib suggests that approximately 10 patients will avoid disease progression events or death in 24 months, and the practice would realize a savings of $733,500.
Conclusions
The NNT model analysis demonstrates that using zanubrutinib to treat R/R CLL patients, compared to acalabrutinib, is associated with more favorable clinical and economic outcomes in the US. Notably, zanubrutinib demonstrated a NNT of 10 to avoid one disease progression or death, along with an estimated cost saving of $7,335 per patient in the US.
Keywords : CLL, NNT, zanubrutinib
Please indicate how this research was funded. : BeOne Medicines Ltd
Please indicate the name of the funding organization.: BeOne Medicines Ltd