Authors
Yi Miao, Ming Liu, Shuchao Qin, Fei Li, Jin Zhang, Hongling Peng, Chunyan Ji, Luomengjia Dai, Ziyuan Zhou, Chongyang Ding, Zhen Wang, Yeqin Sha, Tonglu Qiu, Hanning Tang, Hui Jin, Lei Fan, Wei Xu, Jianyong Li, Yi Xia, Huayuan Zhu.
Introduction
Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) are incurable B-cell malignancy with a heterogeneous clinical course despite advancements in therapies including targeted agents. Ibrutinib combined with fludarabine, cyclophosphamide, and rituximab or obinutuzumab (iFCR or iFCG) in patients with CLL/SLL as first-line therapy demonstrated remarkable efficacy. Orelabrutinib is a novel and highly selective second generation irreversible BTK inhibitor with remarkably less off-target inhibition. This study evaluated the efficacy and safety of the orelabrutinib, fludarabine, cyclophosphamide, and obinutuzumab regimen as the first-line treatment for patients with CLL/SLL without restriction by TP53 aberrations[del(17p) and/or TP53 mutation] and IGHV status.
Methods
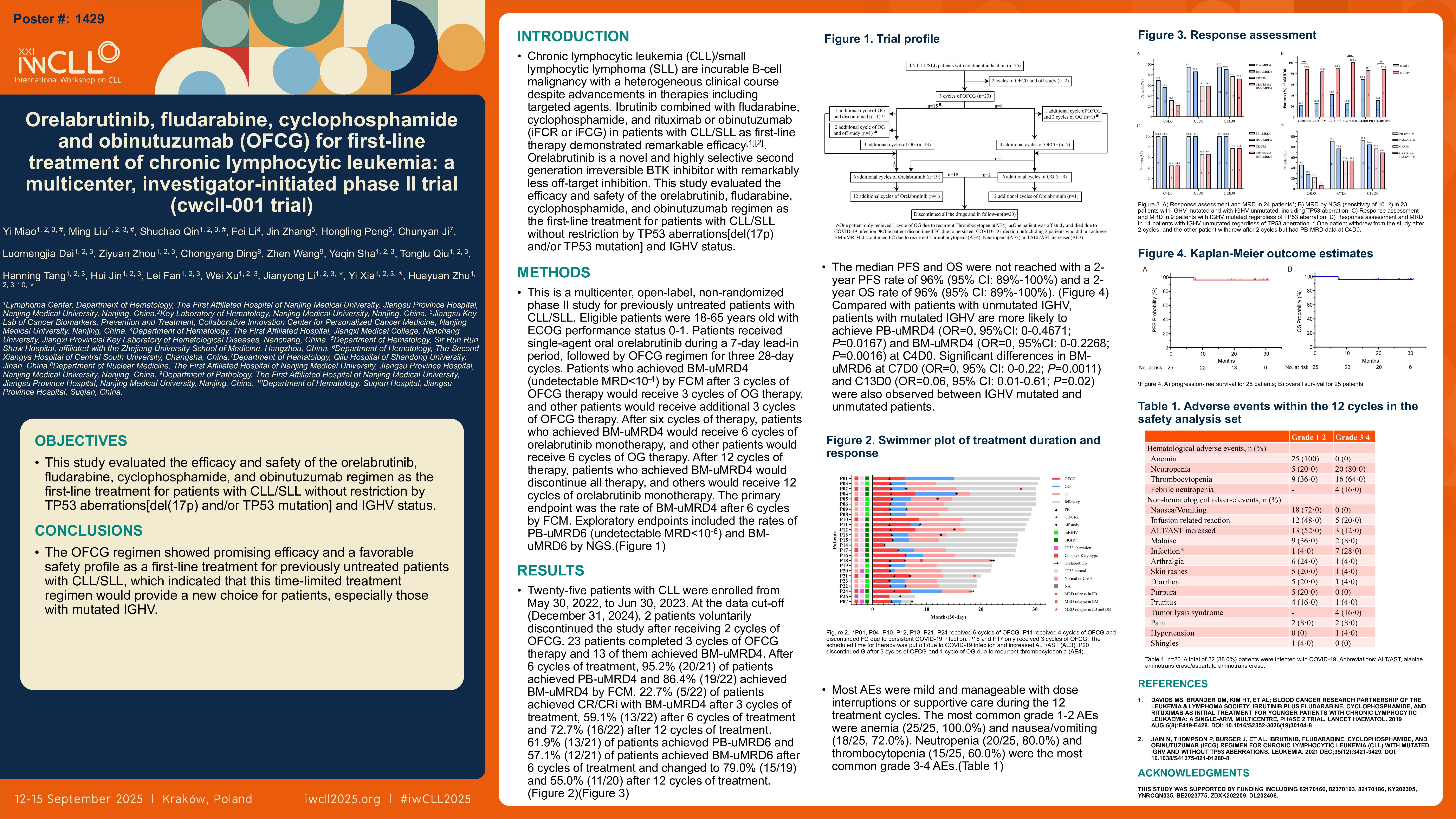
This is a multicenter, open-label, non-randomized phase II study for previously untreated patients with CLL/SLL. Eligible patients were 18-65 years old with ECOG performance status 0-1. Patients received single-agent oral orelabrutinib during a 7-day lead-in period, followed by OFCG regimen for three 28-day cycles. Patients who achieved BM-uMRD4 (undetectable MRD < 10-4) by FCM after 3 cycles of OFCG therapy would receive 3 cycles of OG therapy, and other patients would receive additional 3 cycles of OFCG therapy. After six cycles of therapy, patients who achieved BM-uMRD4 would receive 6 cycles of orelabrutinib monotherapy, and other patients would receive 6 cycles of OG therapy. After 12 cycles of therapy, patients who achieved BM-uMRD4 would discontinue all therapy, and others would receive 12 cycles of orelabrutinib monotherapy. The primary endpoint was the rate of BM-uMRD4 after 6 cycles by FCM. Exploratory endpoints included the rates of PB-uMRD6 (undetectable MRD < 10-6) and BM-uMRD6 by NGS.
Results
Twenty-five patients with CLL were enrolled from May 30, 2022, to Jun 30, 2023. At the data cut-off (December 31, 2024), 2 patients voluntarily discontinued the study after receiving 2 cycles of OFCG. 23 patients completed 3 cycles of OFCG therapy and 13 of them achieved BM-uMRD4. After 6 cycles of treatment, 95.2% (20/21) of patients achieved PB-uMRD4 and 86.4% (19/22) achieved BM-uMRD4 by FCM. 22.7% (5/22) of patients achieved CR/CRi with BM-uMRD4 after 3 cycles of treatment, 59.1% (13/22) after 6 cycles of treatment and 72.7% (16/22) after 12 cycles of treatment. 61.9% (13/21) of patients achieved PB-uMRD6 and 57.1% (12/21) of patients achieved BM-uMRD6 after 6 cycles of treatment and changed to 79.0% (15/19) and 55.0% (11/20) after 12 cycles of treatment. The median follow-up time was 26.8 months (95% CI: 24.9-28.7). The median PFS and OS were not reached with a 2-year PFS rate of 96% (95% CI: 89%-100%) and a 2-year OS rate of 96% (95% CI: 89%-100%). Compared with patients with unmutated IGHV, patients with mutated IGHV are more likely to achieve PB-uMRD4 (OR=0, 95%CI: 0-0.4671; P=0.0167) and BM-uMRD4 (OR=0, 95%CI: 0-0.2268; P=0.0016) at C4D0. Significant differences in BM-uMRD6 at C7D0 (OR=0, 95% CI: 0-0.22; P=0.0011) and C13D0 (OR=0.06, 95% CI: 0.01-0.61; P=0.02) were also observed between IGHV mutated and unmutated patients. Most AEs were mild and manageable with dose interruptions or supportive care during the 12 treatment cycles. The most common grade 1-2 AEs were anemia (25/25, 100.0%) and nausea/vomiting (18/25, 72.0%). Neutropenia (20/25, 80.0%) and thrombocytopenia (15/25, 60.0%) were the most common grade 3-4 AEs.
Conclusions
The OFCG regimen showed promising efficacy and a favorable safety profile as a first-line treatment for previously untreated patients with CLL/SLL, which indicated that this time-limited treatment regimen would provide a new choice for patients, especially those with mutated IGHV. Given these data, a larger randomized controlled trial is needed in the future to validate these findings.
Keywords : CLL/SLL, Combination therapy, Clinical trials
Please indicate how this research was funded.:
Please indicate the name of the funding organization. :