Authors
Adam S. Kittai, Paul J. Hampel, Joanna M. Rhodes, Xiaoliang Wang, Qianhong Fu, Danni Zhao, Smriti Karwa, Taavy A. Miller, Olive Mbah, Ahmed Sawas, Benji Wagner, Rachel Myers, Derrick van Beuge, Gregory A. Maglinte, Erlene K. Seymour, Jacqueline C. Barrientos.
Background
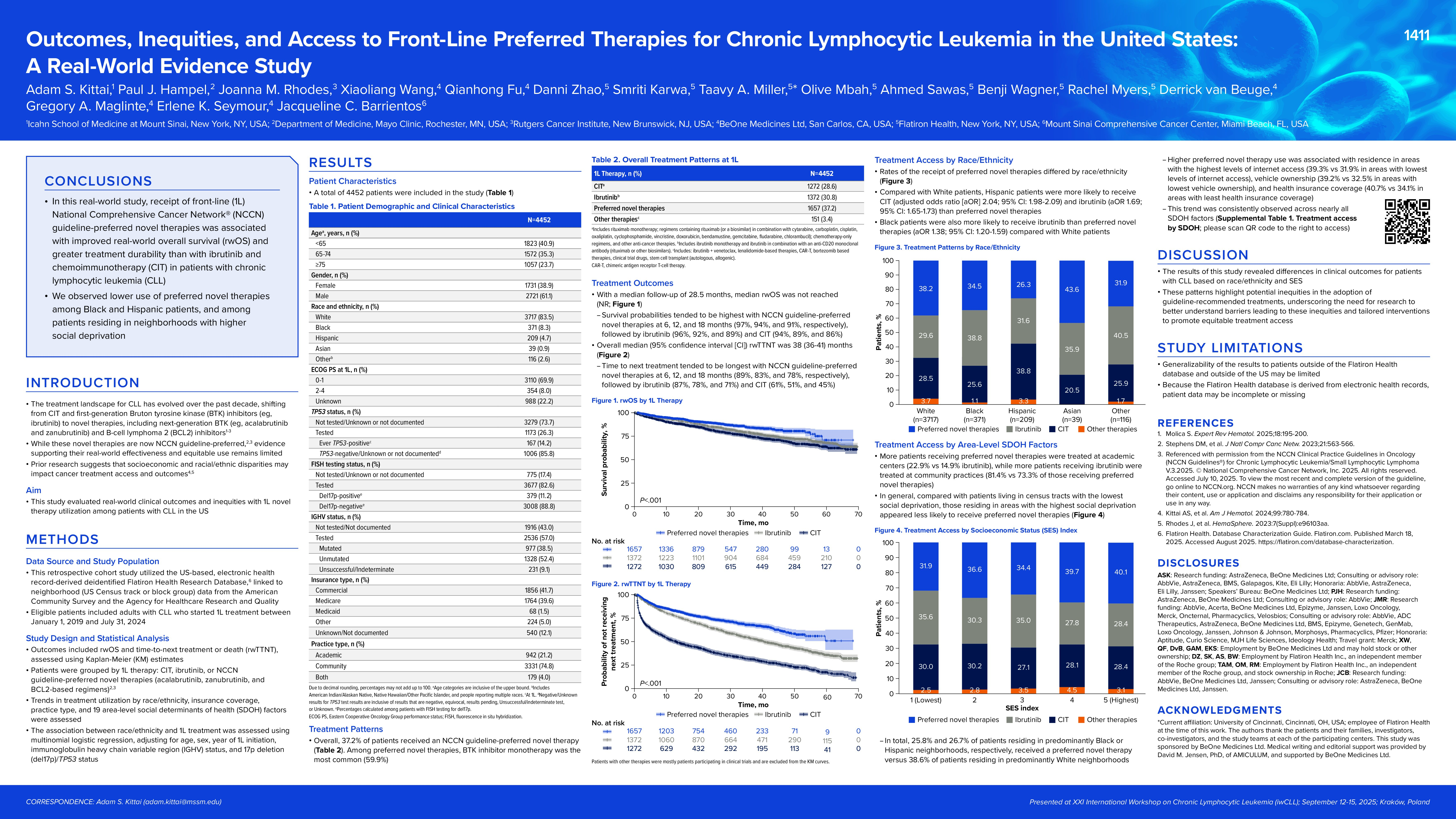
The treatment landscape for chronic lymphocytic leukemia (CLL) has evolved over the past decade, shifting from chemoimmunotherapy (CIT) and first-generation Bruton tyrosine kinase (BTK) inhibitors (eg, ibrutinib) to next-generation BTK and B-cell lymphoma 2 (BCL2) inhibitors. While these novel therapies (NTs) are now National Comprehensive Cancer Network® (NCCN) guideline–preferred, evidence supporting their real-world effectiveness and equitable use remains limited. Prior research suggests that socioeconomic and racial/ethnic disparities may impact cancer treatment access and outcomes. We evaluated real-world clinical outcomes and inequities with front-line (1L) NT utilization among patients with CLL in the US.
Methods
This retrospective cohort study utilized the US-based, electronic health record-derived deidentified Flatiron Health Research Database, linked to neighborhood (US Census track or block group) data from multiple sources. Eligible patients included adults with CLL who started 1L treatment between 01/01/2019 and 07/31/2024. Outcomes included real-world overall survival (rwOS) and time-to-next treatment or death (rwTTNT), assessed using Kaplan-Meier estimates. Patients were grouped by 1L therapy: CIT, ibrutinib, or NCCN guideline–preferred NTs (acalabrutinib, zanubrutinib, and BCL2-based regimens). Trends in treatment utilization by race/ethnicity, insurance, practice type, and 18 area-level social determinants of health factors were assessed. Association between race/ethnicity and 1L treatment was assessed using multinomial logistic regression, adjusting for age, sex, year of 1L initiation, IGHV, and del17p/TP53 status.
Results
Of the 4452 patients included in the study, 3717 were White (83%), 371 were Black (8%), 209 were Hispanic (5%), and 155 were Other race (4%; includes Asian, American Indian/Alaska Native, Native Hawaiian/Other Pacific Islander, and people reporting multiple races). Overall, 37% of patients received an NCCN guideline–preferred NT (eg, acalabrutinib, zanubrutinib, BCL2-based regimens). Among preferred NTs, BTK inhibitor monotherapy was used the most often (60%).
At a median follow-up of 28.5 months, median rwOS was not reached (NR). Survival probabilities tended to be highest with NCCN guideline–preferred NTs at 6, 12, and 18 months (97%, 94%, and 91%, respectively), followed by ibrutinib (96%, 92%, and 89%) and CIT (94%, 89%, and 86%). Median rwTTNT was NR in patients receiving a preferred NT; the median rwTTNT in patients receiving ibrutinib was 40 months (95% CI 37-45) and in those receiving CIT was 13 months (95% CI 11-15).
The receipt of preferred NTs was highest among White (38%), followed by Other (35%), Black (34%), and Hispanic (26%) patients. More patients receiving preferred NTs were treated at academic centers (23% vs 15% ibrutinib), while more patients receiving ibrutinib were treated at community practices (73% preferred NTs vs 81% ibrutinib). In general, compared with patients living in census tracts with the lowest social deprivation, those residing in areas with the highest social deprivation appeared less likely to receive preferred NTs. Among those residing in areas with the highest socioeconomic status (SES) index, 40% received preferred NTs versus only 32% of patients residing in areas with the lowest SES index. In total, 26% and 27% of patients residing in predominantly Black or Hispanic neighborhoods, respectively, received a preferred NT versus 39% of patients residing in predominantly White neighborhoods. Higher NT use also seemed to be associated with residence in areas with the highest levels of internet access (39% vs 32% in areas with lowest levels of internet access), vehicle ownership (39% vs 33% in areas with lowest vehicle ownership), and health insurance coverage (41% vs 34% in areas with least health insurance coverage).
Compared with White patients, Hispanic patients were more likely to receive CIT (adjusted odds ratio [aOR] 2.04; 95% CI 1.98-2.09) and ibrutinib (aOR 1.69; 95% CI 1.65-1.73) than preferred NTs. Black patients were also more likely to receive ibrutinib than preferred NTs (aOR 1.38; 95% CI 1.20-1.59) compared with White patients.
Conclusion
Receipt of 1L NCCN guideline–preferred NTs was associated with better real-world survival and treatment durability compared with ibrutinib and CIT among patients with CLL. We observed lower use of preferred NTs among Black and Hispanic patients, and among patients residing in neighborhoods with higher social deprivation. These patterns highlight potential inequities in the adoption of guideline-recommended treatments, underscoring the need for research to better understand barriers leading to these inequities and tailored interventions to promote equitable treatment access.
Keywords : Racial disparities, front-line treatment patterns, outcomes
Please indicate how this research was funded. : This study is funded by BeOne Medicines Ltd.
Please indicate the name of the funding organization.: BeOne Medicines Ltd.