Prevalence of BTK, PLCG2, and BCL2 mutations in CLL patients in Croatia – KROHEM study (969kB pdf)
Authors
Branimir Gizdić, Ivona ArićZrna, Mia NižetićGović, Petra Veić, Barbara Dreta, Inga Mandac Smoljanović, Sandra Bašić Kinda, Renata BabokFlegarić, Hana Mažbrada, Dragana Grohovac, Martina Marjanović, Jasminka Sinčić-Petričević, Ena Sorić, Marija IvićČikara, Vlatko Pejša, Igor Aurer, OzrenJakšić.
Introduction
Targeted therapies in Chronic Lymphocytic Leukemia (CLL), including Bruton tyrosine kinase inhibitors (BTKi) and Bcl-2 antagonists (Bcl2a), have led to significant improvements in outcomes for both treatment-naive (TN) and relapsed/refractory (RR) patients. These therapies are now standard options for almost all CLL patients (ESMO, KROHEM). However, high-risk molecular features of the disease, such as TP53 aberrations (del17p and/or TP53 mutations), are still linked to inferior outcomes and guide therapeutic decisions. Testing for these features (by FISH and sequencing) before each line of therapy is a standard recommendation. In relapsed/refractory patients previously treated with BTKi and/or BCL2a, resistance mutations in BTK and PLCG2 and/or BCL2 have been described, respectively. However, testing for these mutations is still not part of routine practice.
Methods
Since September 2023, all CLL patients in Croatia whose samples are tested for TP53 mutation are also tested by NGS (with sensitivity 1%) using a customized panel that includes BTK, PLCG2, and BCL2 genes along with TP53 (exon2-11). To evaluate the prevalence of BTK, PLCG2, and BCL2 mutations among TP53 mutation-tested patients and their relation to treatment status, treatment data for CLL patients tested from 8 centers were retrospectively collected, while all mutation analyses were performed in one laboratory. Routine practice is to test all patients for TP53 mutation before each treatment line unless del17p was detected by FISH, or the reason for treatment change is adverse events.
Results
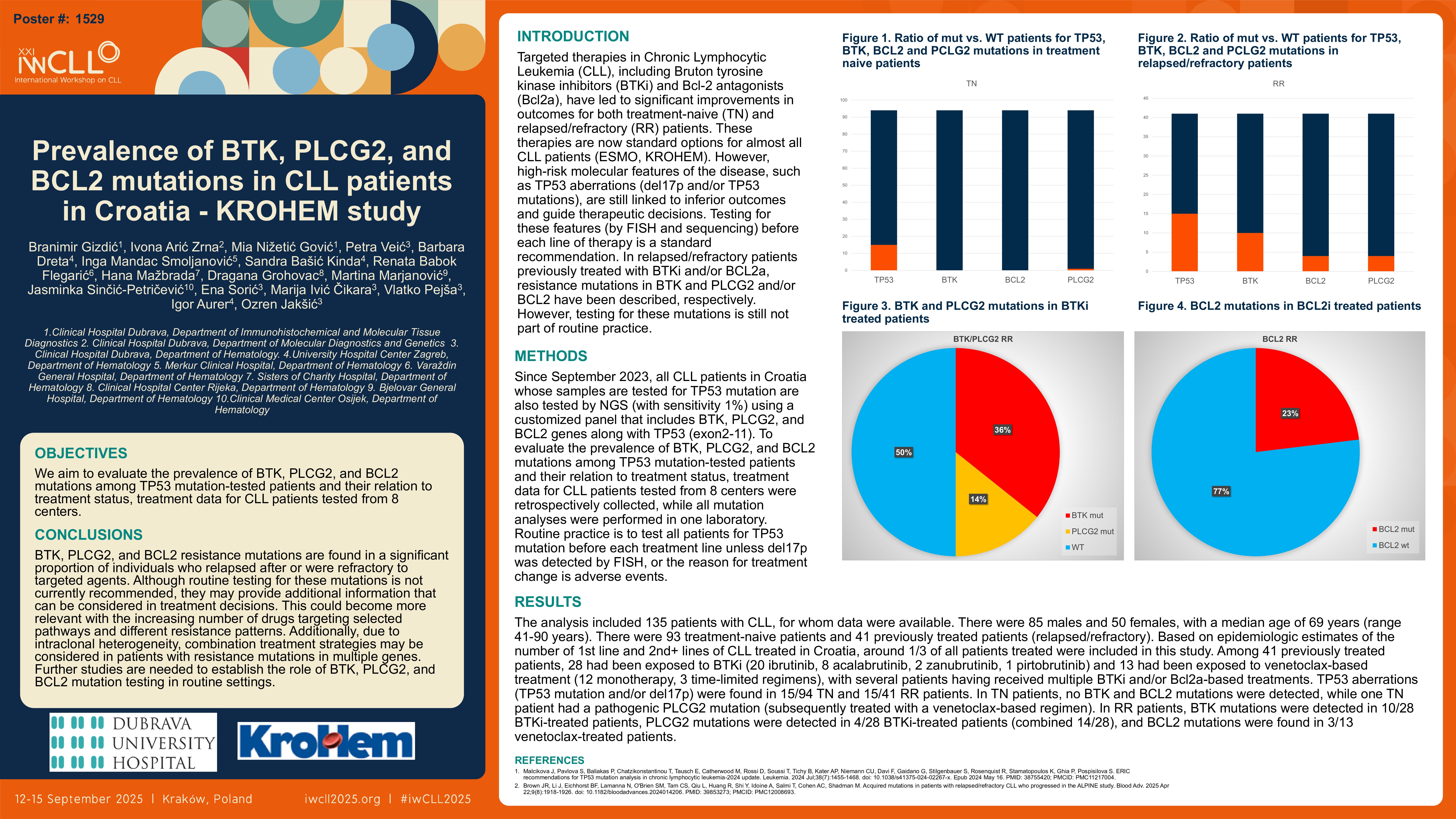
The analysis included 135 patients with CLL, for whom data were available. There were 85 males and 50 females, with a median age of 69 years (range 41-90 years). There were 93 treatment-naive patients and 41 previously treated patients (relapsed/refractory). Based on epidemiologic estimates of the number of 1st line and 2nd+ lines of CLL treated in Croatia, around 1/3 of all patients treated were included in this study. Among 41 previously treated patients, 28 had been exposed to BTKi (20 ibrutinib, 8 acalabrutinib, 2 zanubrutinib, 1 pirtobrutinib) and 13 had been exposed to venetoclax-based treatment (12 monotherapy, 3 time-limited regimens), with several patients having received multiple BTKi and/or Bcl2a-based treatments. TP53 aberrations (TP53 mutation and/or del17p) were found in 15/94 TN and 15/41 RR patients. In TN patients, no BTK and BCL2 mutations were detected, while one TN patient had a pathogenic PLCG2 mutation (subsequently treated with a venetoclax-based regimen). In RR patients, BTK mutations were detected in 10/28 BTKi-treated patients, PLCG2 mutations were detected in 4/28 BTKi-treated patients (combined 14/28), and BCL2 mutations were found in 3/13 venetoclax-treated patients.
Conclusions
BTK, PLCG2, and BCL2 resistance mutations are found in a significant proportion of individuals who relapsed after or were refractory to targeted agents. Although routine testing for these mutations is not currently recommended, they may provide additional information that can be considered in treatment decisions. This could become more relevant with the increasing number of drugs targeting selected pathways and different resistance patterns. Additionally, due to intraclonal heterogeneity, combination treatment strategies may be considered in patients with resistance mutations in multiple genes. Further studies are needed to establish the role of BTK, PLCG2, and BCL2 mutation testing in routine settings.
Keywords : leukemia, relapsed/refractory, biomarker
Please indicate how this research was funded. :
Please indicate the name of the funding organization