Authors
Vanthana Bharathi, Lili Zhou, Ayad K. Ali, Qianhong Fu, Wassim Aldairy, Alessandra Ferrajoli.
Background
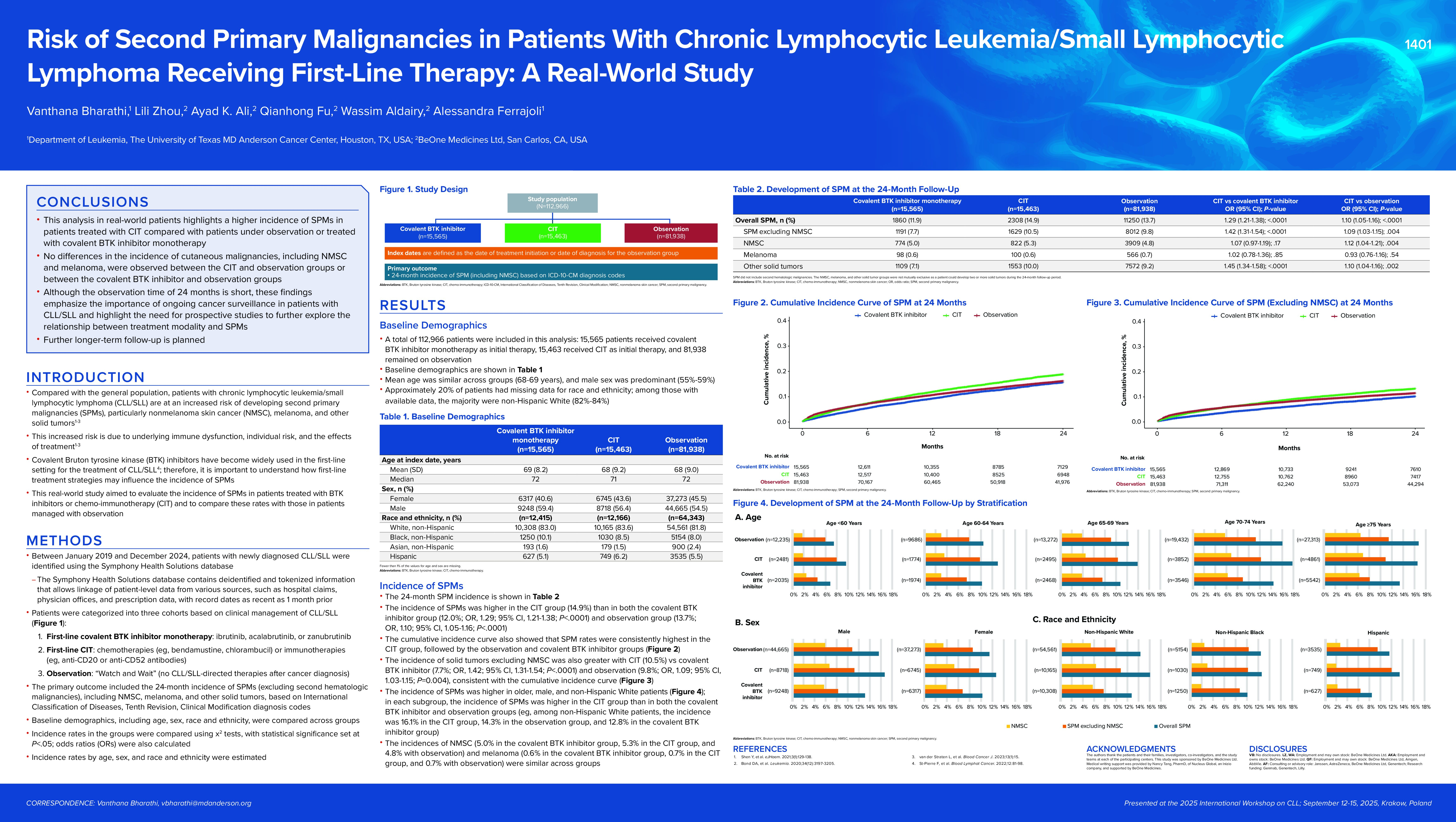
Patients with CLL/SLL are at increased risk of developing second primary malignancies (SPM) due to underlying immune dysfunction, individual risk, and the effects of treatment. Covalent Bruton tyrosine kinase inhibitors (cBTKi) have become widely used in the first-line setting for treatment of CLL/SLL. Therefore, it is important to understand how first-line treatment strategies influence the incidence of SPM. Our study aimed to evaluate the real-world incidence of SPM in patients treated with BTKi or chemo- immunotherapy (CIT) and to compare these rates with those in patients managed with observation.
Methods
Between January 2019 and December 2024, patients with newly diagnosed CLL/SLL were identified using the Symphony Health Solutions database. Patients were categorized into three cohorts based on clinical management: (1) patients receiving first-line treatment with cBTKi monotherapy (ibrutinib, acalabrutinib, or zanubrutinib); (2) patients receiving first-line treatment with CIT; and (3) patients managed with observation. The index date was defined as the date of treatment initiation or date of diagnosis for the observation group. Outcomes included the 24-month incidence of SPM (including non-melanoma skin cancer (NMSC)) based on ICD-10-CM diagnosis codes. Baseline demographics, including age, gender, and race/ethnicity were compared across cohorts.
Results
A total of 112,966 patients were included in this analysis. 15,565 patients received cBTKi as initial therapy; 15,463 patients received CIT as initial therapy; and 81,938 patients remained on observation. Mean age across cohorts was 68–69 years; approximately 55–59% were male. The 24-month incidence of SPM was 12.0% in patients treated with cBTKi, 14.9% in patients treated with CIT, and 13.7% in patients that remained on observation. The incidence of solid tumors excluding NMSC was 7.7% (cBTKi cohort), 10.5% (CIT cohort), and 9.8% (observation cohort). The incidence of skin malignancies was reviewed and NMSC were observed in 5.0% of patients treated with cBTKi, 5.3% of patients treated with CIT, and 4.8% of patients that remained on observation, the incidence of melanoma was in 0.6% in the cBTKi cohort, 0.7% in the CIT cohort, and 0.7% in the observation cohort. Compared to patients that remained on observation, SPM were less frequent with cBTKi (OR=0.86, 95% CI: 0.82–0.91, p< 0.001) and more frequent with CIT (OR=1.10, 95% CI: 1.05–1.16, p< 0.001).
Conclusions
This analysis of real-world patients highlights a higher incidence of SPM in patients treated with CIT compared to patients of observation or those treated with cBTKi. No differences in the incidence of cutaneous malignancies including NSMC and melanoma were observed between patients treated with CIT and patients on observation and between patients treated with BTKi and patients on observation. Although the observation time of 24 months is short and a longer follow-up is planned, these findings emphasize the importance of ongoing cancer surveillance in patients with CLL/SLL and highlight the need for prospective studies to further explore the relationship between treatment modality and SPM.
Keywords : chemo- immunotherapy, cBTKi, second primary malignancies
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: BeOne Medicines Ltd