Authors
Alessandra Tedeschi, Anders Österborg, Talha Munir, Patricia A. Walker, Tadeusz Robak, Hanna Ciepluch, Richard Greil, Tian Tian, Marcus Lefebure, Jamie Hirata, Constantine S. Tam
Introduction
Chronic lymphocytic leukemia (CLL) commonly affects the elderly, with a median age of diagnosis of 72 years (Eichhorst B, et al. Ann Oncol 2015). In these patients, comorbidities and suboptimal performance status may limit the efficacy of newer therapeutic interventions. In the Phase 3 SEQUOIA study (NCT03336333), zanubrutinib, a highly potent and selective next-generation Bruton tyrosine kinase inhibitor, demonstrated a superior safety and efficacy profile compared with bendamustine + rituximab (BR) in treatment-naïve patients with CLL/small lymphocytic lymphoma (SLL). Furthermore, patients with del(17p) treated with zanubrutinib have achieved high overall response rates (ORR) and progression-free survival (PFS). This subgroup analysis aimed to assess the safety and efficacy of zanubrutinib vs BR in older (≥75 years) patients.
Methods
SEQUOIA enrolled treatment-naive patients with CLL/SLL. Cohort 1 included patients without del(17p) randomized 1:1 to receive zanubrutinib or BR; Cohort 2 included patients with del(17p) assigned to receive zanubrutinib. Patients included in this analysis were restricted by age ≥75 years (elderly).
Results
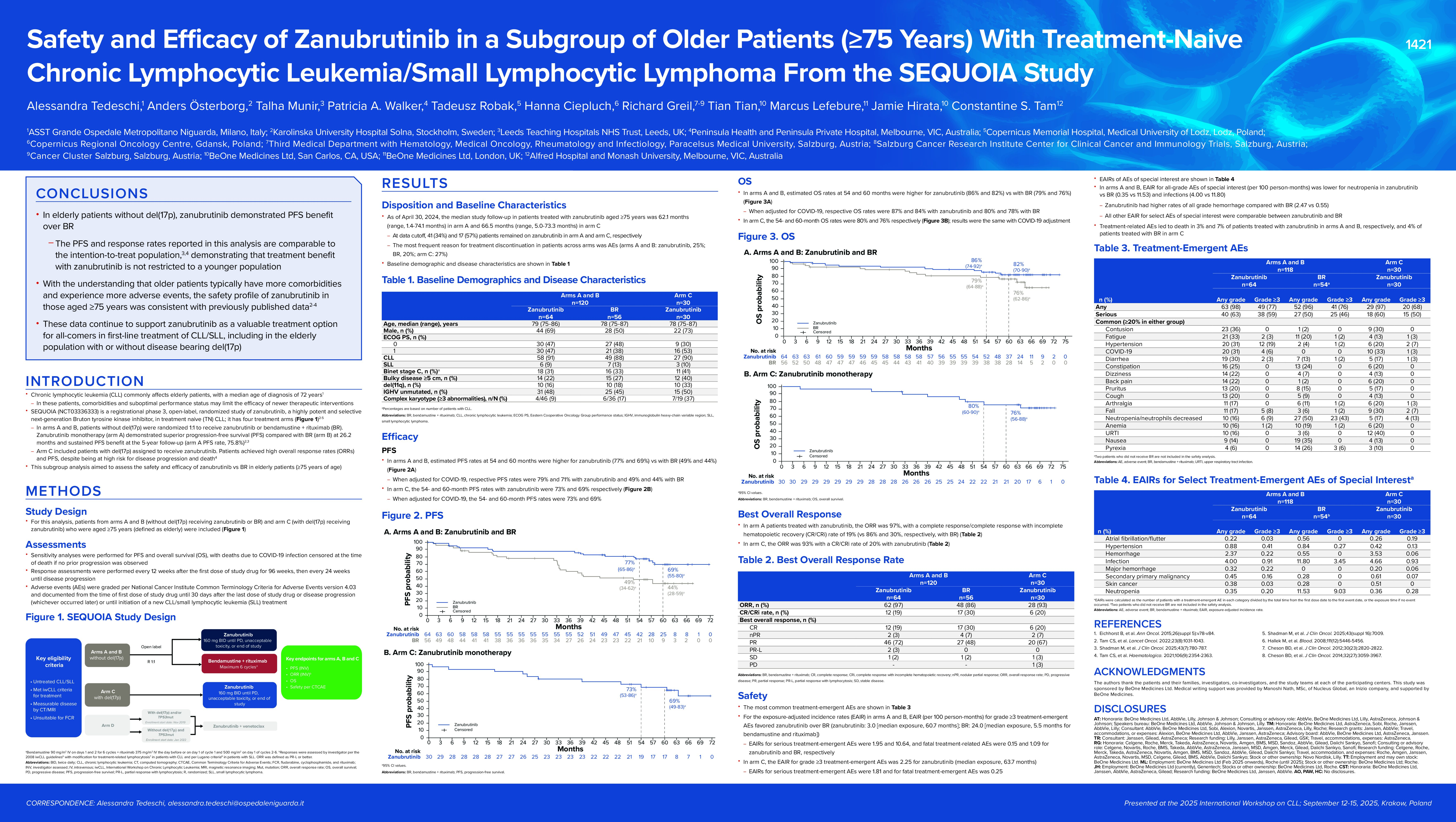
As of April 30, 2024, the median study follow-up for patients aged ≥75 years was 62.1 (range, 1.4-74.1) months for Cohort 1 and 66.5 (range, 5.0-73.3) months in Cohort 2. In Cohort 1, 120 patients were aged ≥75 years, 56 patients received BR and 64 patients received zanubrutinib; median age was 78 (range, 75-87) years. Cohort 2 had 30 patients aged ≥75 years.
In Cohort 1 patients treated with zanubrutinib, the ORR was 97%, with a complete response/complete response with incomplete hematopoietic recovery (CR/CRi) rate of 19% (vs 86% and 30%, respectively, with BR). Estimated PFS rates (95% CI) at 54 and 60 months were 77% (65%-86%) and 69% (55%-80%), respectively, with zanubrutinib and 49% (34%-62%) and 44% (28%-59%) with BR. When adjusted for COVID-19, zanubrutinib PFS rates were 79% (66%-87%) and 71% (56%-81%), and BR rates were 49% (34%-62%) and 44% (28%-59%). Estimated OS rates (95% CI) at 54 and 60 months were 86% (74%-92%) and 82% (70%-90%), respectively, with zanubrutinib and 79% (64%-88%) and 76% (62%-86%) with BR. When adjusted for COVID-19, zanubrutinib OS rates were 87% (76%-93%) and 84% (72%-91%), and BR rates were 80% (66%-89%) and 78% (64%-87%).
In Cohort 2, the ORR was 93% with a CR/CRi rate of 20% with zanubrutinib. The 54- and 60-month PFS rates (95% CI) were 73% (53%-86%) and 69% (49%-83%), respectively, with and without adjustment for COVID-19; the 54- and 60-month OS rates were 80% (60%-90%) and 76% (56%-88%). In Cohort 1, grade ≥3 adverse events (AEs) were observed in 77% with zanubrutinib and 89% with BR; serious AEs (SAEs) occurred in 64% and 65% of patients, respectively. In Cohort 2, the rates of grade ≥3 AEs and SAEs were 67%, and 63%, respectively. Key AEs of special interest (AESI, any grade/grade ≥3) in Cohort 1 patients treated with zanubrutinib included atrial fibrillation/flutter (11%/2%), bleeding (59%/11%), and hypertension (34%/19%); with BR, rates of these AESI were 4%/0%, 4%/0%, and 6%/2%, respectively. AESI (any grade/grade ≥3) in Cohort 2 patients treated with zanubrutinib included atrial fibrillation/flutter (13%/10%), bleeding (67%/3%), and hypertension (20%/7%). AEs led to death in 9% and 13% of patients treated with zanubrutinib in Cohorts 1 and 2, respectively, and 17% of patients treated with BR in Cohort 1. In Cohorts 1 and 2, 64% and 57% remained on zanubrutinib at data cutoff, respectively. The most frequent reason for treatment discontinuation in patients across cohorts was AEs (Cohort 1: zanubrutinib, 25% and BR, 20%; Cohort 2: 27%).
Conclusion
In this subgroup analysis, the efficacy of zanubrutinib was largely comparable for elderly patients with and without disease harboring del(17p). In elderly patients without del(17p), zanubrutinib demonstrated PFS benefit over BR. The PFS and response rates reported in this analysis are comparable to published data in the intention-to-treat population, demonstrating that treatment benefit with zanubrutinib is not restricted to a younger population. With the understanding that older patients typically have more comorbidities and experience more AEs, the safety profile of zanubrutinib in those aged ≥75 years was consistent with previously published data. These data continue to support zanubrutinib as a valuable treatment option for all-comers in the first-line CLL/SLL setting, including the elderly population with or without disease bearing del(17p).
Keywords : Zanubrutinib, CLL, Elderly
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: BeOne Medicines Ltd