Setting a 3D model to study Chronic Lymphocytic Leukemia (1MB pdf)
Authors
Martina Pasino, Chiara Gentili, Fabrizio Loiacono, Irena Velkova and Paola Menichini.
Background
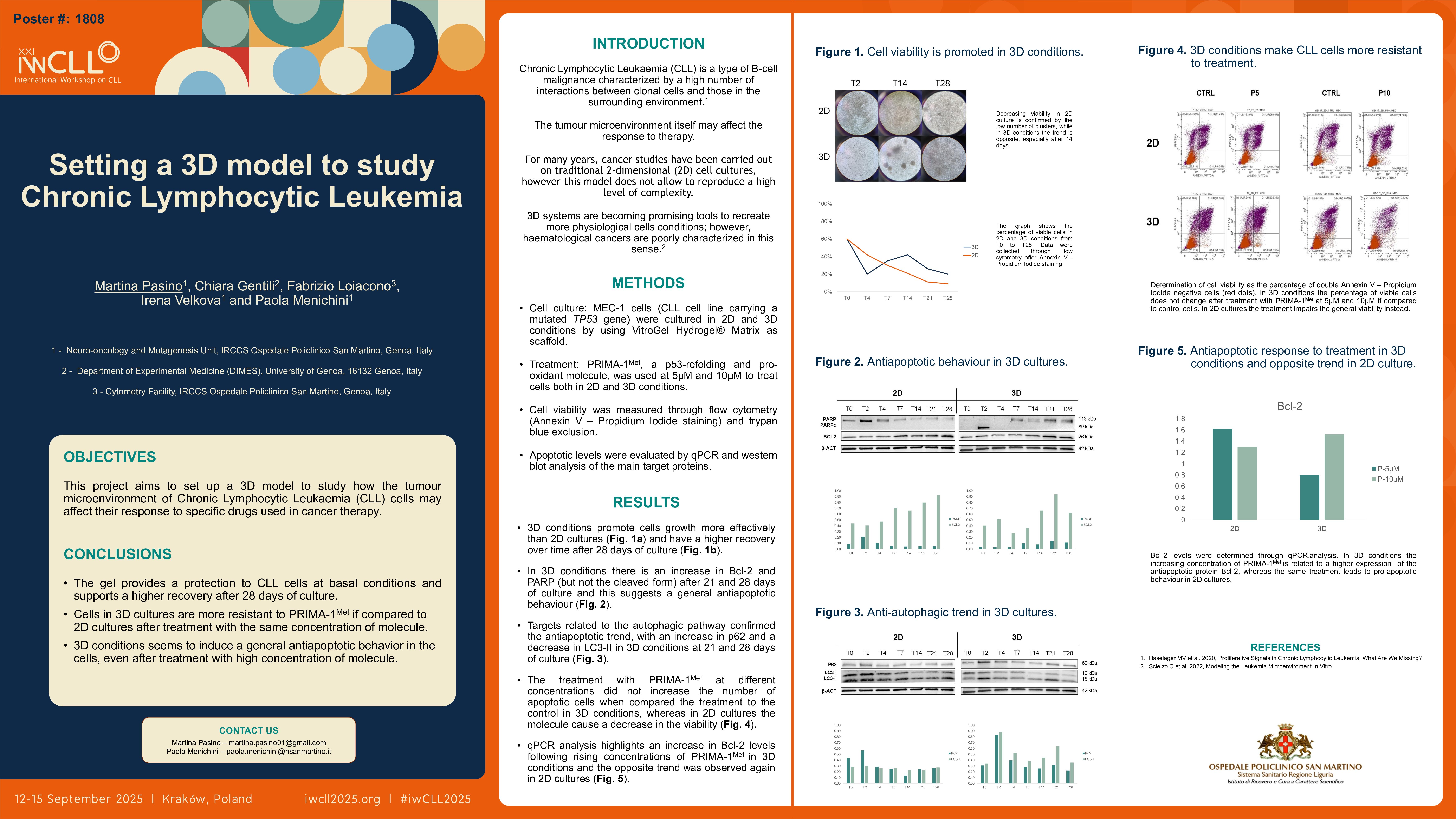
The tumour microenvironment plays a crucial role in promoting survival and proliferation of malignant cells. Traditional 2D culture does not allow for recreating this level of complexity; thus, 3D systems are becoming promising tools for recreating more physiological cell conditions. While 3D cultures of solid tumours are more commonly set up, haematological cancers are poorly characterized in this sense. This project aims to create a 3D model to investigate how the tumour microenvironment of Chronic Lymphocytic Leukaemia (CLL) cells may influence their response to specific drugs used in cancer therapy.
Methods
VitroGel Hydrogel® Matrix, a ready-to-use, animal-origin-free functional hydrogel, was used as a scaffold to test different culture conditions of MEC-1 human CLL cell lines. Cell viability was measured through trypan blue exclusion, flow cytometry and annexin V-propidium iodide staining. Western blot analysis was used to detect the levels of different proteins involved in the apoptotic pathway (i.e., Bcl-2, PARP), and qPCR was performed to determine the expression of genes related to apoptosis, migration, and proliferation pathways.
Results
We first plated MEC-1 cells in 3D and 2D conditions, and observed higher viability in 3D after 28 days of culture compared to 2D cells. Despite the high mortality rate in 3D conditions during the first week of culture, 3D cells showed good recovery over time. On the other hand, 2D culture appears to facilitate better survival initially, whereas viability begins to decrease after 7 days of culture. The anti-apoptotic trend was confirmed in 3D conditions by Western blot analysis: in 3D cells, we observed an increase in Bcl-2 and PARP (but not the cleaved form) after 21 and 28 days of culture. This suggests a general antiapoptotic behaviour. We also investigated autophagy, and we detected an increase in p62 and a decrease in LC3-II in 3D conditions at 21 and 28 days of culture. 2D cells exhibited a general opposite trend, which is consistent with the decreased cell viability observed after three weeks of culture. We then decided to treat cells with PRIMA-1Met, a p53-refolding and pro-oxidant molecule, to investigate whether the presence of the scaffold can increase cell resistance even after treatment. We observed no differences in cell viability between control and treated cells in 3D cultures, while in 2D conditions the molecule kills the cells. The qPCR analysis highlights an increase in Bcl-2 levels following rising concentrations of PRIMA-1Met (from 5 μM to 40 μM) in 3D conditions and the opposite trend was observed in 2D cultures. We also evaluated the expression of genes related to cytoskeleton remodelling and migration, but these aspects still further evaluation.
Conclusions
These preliminary results indicate that the gel seems to provide protection to CLL cells both in normal conditions and after treatment with PRIMA-1Met. This is probably related to the cell-scaffold interaction, which recreates a more physiological environment than 2D cultures. Based on these results, we will exploit this model to test new combinations of drugs already used in clinical practice to treat CLL. We will also apply this model to study primary CLL cells, aiming to enhance cell survival and assess the actual effects of various drugs under more physiological conditions.
Keywords : Leukemia, 3D
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: