Authors
Maria L. Andersson, Olina Lind, Kia Heimersson, Anna Berglöf, Teresa Del Peso Santos, Lucia Peña Perez, Qing Wang, Tom A. Mulder, Rula Zain, Robert Månsson, Richard Rosenquist, C.I. Edvard Smith, Anders Österborg and Marzia Palma.
Background
The covalent Bruton tyrosine kinase inhibitors acalabrutinib and zanubrutinib are preferred as single-agent treatment in clinical practice for patients with chronic lymphocytic leukemia (CLL) due to their high efficacy and improved safety profiles compared to the first-in-class ibrutinib. Despite enhanced kinase selectivity, their long-term immunomodulatory effects remain incompletely characterized. We conducted a longitudinal study to compare the biological effects of acalabrutinib and zanubrutinib on CLL tumor cell fractions, immune cell composition and plasma protein biomarkers.
Methods
Peripheral blood samples from 34 CLL patients treated with either acalabrutinib (n=18) or zanubrutinib (n=16) were collected at multiple time points over a 24-month (mo) period. Immune monitoring included flow cytometry and proximity extension assay (Olink) to assess immune cell subsets and 92 inflammatory plasma proteins. Tumor cell subpopulations were classified into proliferative (PF, CD5^bright CXCR4^dim) and resting (RF, CD5^dim CXCR4^bright) fractions. ddPCR was performed to detect BTK hotspot mutations. Clinical outcomes were recorded, and age- and sex-matched healthy donors (HD) served as controls.
Results
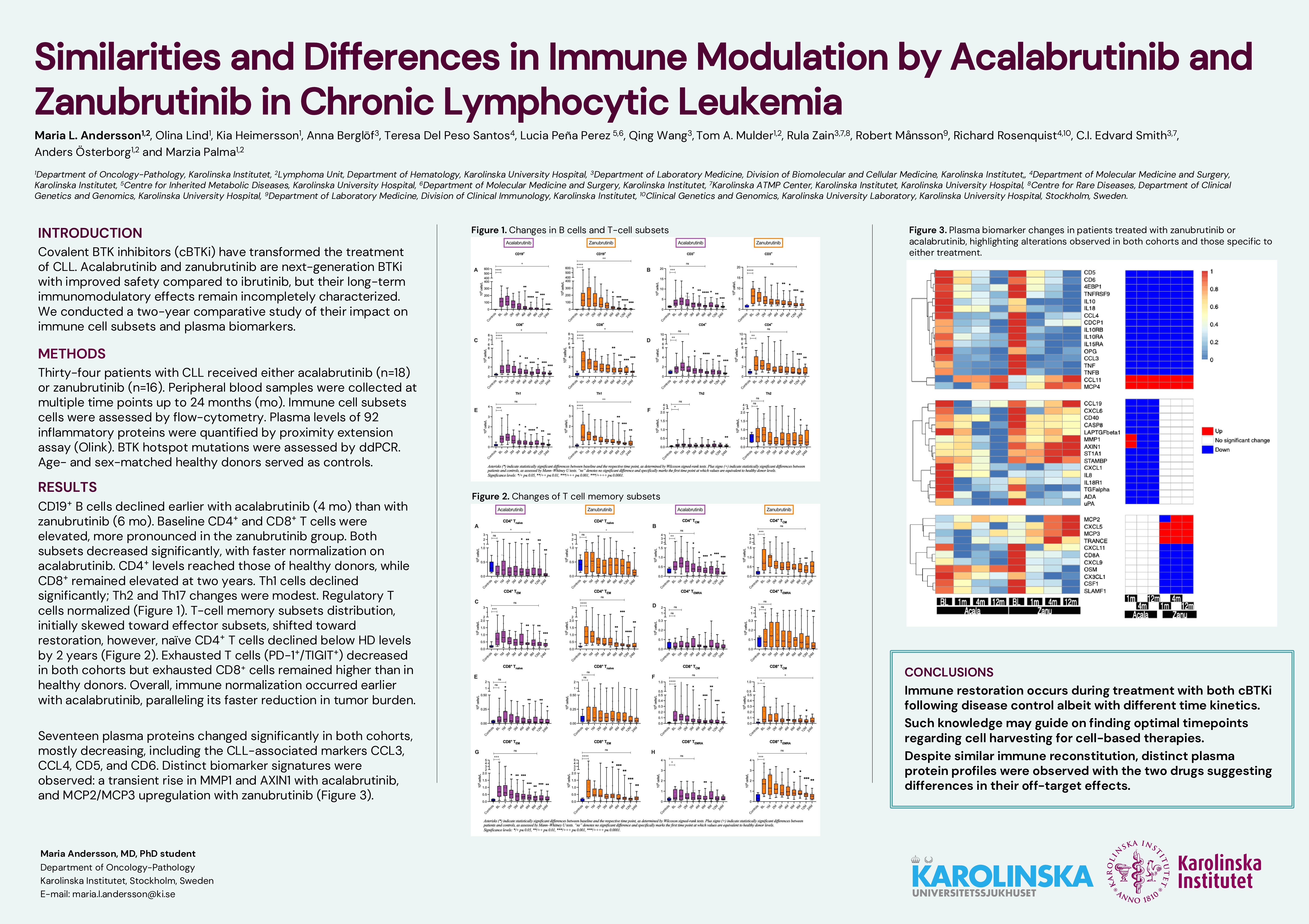
B cell (CD19+) counts declined as expected during the treatment in both cohorts, with a significant reduction vs baseline occurring earlier in the acalabrutinib cohort (2 mo) compared to the zanubrutinib cohort (6 mo). Analysis of tumor fractions revealed a reduction in the PF population during early treatment, followed by a plateau or slight increase at later time points. Two patients in the zanubrutinib group had high PF at the 2-year follow-up and within a month both had progressive disease. RF showed an initial rise but decreased by month 24 in the acalabrutinib cohort.
At baseline both cohorts exhibited elevated CD4⁺ and CD8⁺ T cell counts, more pronounced in the zanubrutinib group. Both subsets decreased significantly in both cohorts at mo 3 in the acalabrutinib cohort and mo 4–6 in the zanubrutinib cohort. While CD4⁺ T cells reached HD levels, CD8⁺ T cells remained elevated at the final 2-year follow-up. T cell memory subsets distribution, initially skewed toward effector subsets, shifted toward restoration, however, naïve CD4⁺ T cells declined below HD levels by 2 years. Th1 cells decreased significantly during treatment in both cohorts; Th2 and Th17 cell changes were less marked. Regulatory T cells (Tregs) declined early in both cohorts and normalized. Exhausted T cells (PD-1⁺/TIGIT⁺) decreased during therapy but remained partially elevated compared to HD. Most T-cell subsets declined and normalized faster during treatment with acalabrutinib compared to zanubrutinib, which paralleled with a faster reduction of the circulating tumor burden (i.e. CD19+ cells).
Of the 92 plasma biomarkers assessed, 17 changed significantly in both cohorts—mostly decreasing—including CLL-associated markers CCL3, CCL4, CD5, and CD6. Acalabrutinib uniquely altered 15 biomarkers, including a transient increase in MMP1 and AXIN1 at 1 month. Zanubrutinib selectively modulated 11 markers, including upregulation of the monocyte chemoattractant proteins MCP2 and, MCP3.
Conclusion
Acalabrutinib and zanubrutinib both induce substantial immune modulation and reductions in tumor-associated biomarkers in CLL. Despite similarities in immune cell kinetics, distinct plasma protein profiles were observed with the two drugs suggesting differences in their off-target effects.
Keywords : cBTKi, T cells, biomarkers
Please indicate how this research was funded. : This work was supported by grants from the Swedish Blood Cancer Association, the Swedish Cancer Foundation, the Swedish Research Council, King Gustav V Jubilee Fund, the Stockholm County Council, and the Center for Innovative Medicine (CIMED), and by unrestricted research grants by Beigene LDT and Astra Zeneca.
Please indicate the name of the funding organization.: