Authors
Britten K. Gordon, Lillian M. Cool, Elizabeth Muhowski, Lianbo Yu, Janani Ravikrishnan, Samon Benrashid, Andrew Mitchell, Alexander He, Shrilekha Misra, Tzung-Huei Lai, Shanmugapriya Thangavadivel, Alexander Marr, Jazmin Urrutia, Casey Leimbach, Naina Karnati, Serena Li Zhao, Sonam Sonam, Smita Kumari, Elizabeth Perry, Kerry A. Rogers, Adam S. Kittai, Seema A. Bhat, Aseel Alsouqi, Natarajan Muthusamy, John C Byrd, Deepa Sampath, Rosa Lapalombella, Blake R. Peterson, Yi Chen, Fenlai Tan, Stephen P. Anthony, Yu Chen, Jennifer A. Woyach.
Background
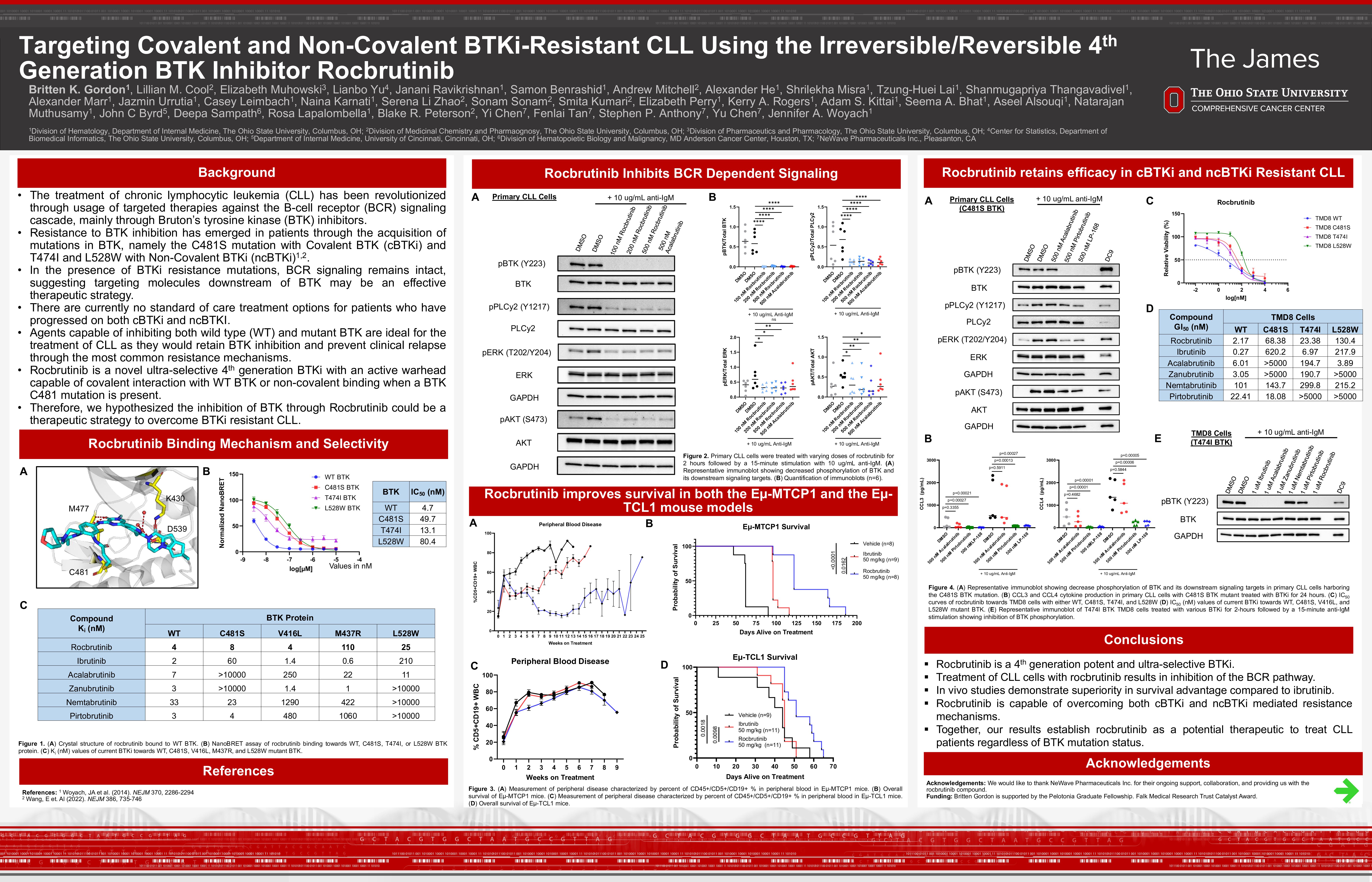
Treatment of chronic lymphocytic leukemia (CLL) has been transformed by targeted therapies including inhibitors of Bruton’s tyrosine kinase (BTKi). Currently three covalent BTKi (cBTKi) are approved for CLL, but most patients eventually relapse, commonly through acquisition of the C481S BTK mutation (Woyach et al., 2014). Non-covalent BTKi (ncBTKi), retain activity against C481 mutations but are susceptible to secondary BTK mutations (T474I, L528W, M427R, and V416L), which can also confer resistance to covalent BTKi (Wang et al., 2022). Regardless of these mutations, BCR signaling remains intact, suggesting that inhibition of the BCR pathway retains its therapeutic importance. Agents capable of targeting and inhibiting both wild-type (WT) and mutant BTK (C481S, T474I, and L528W) are ideal for treating CLL as they would retain BTK inhibition and prevent clinical relapse through the most common resistance mechanisms. Rocbrutinib is a novel selective 4th generation BTKi with an active warhead capable of binding WT and mutant BTK.
Methods
Validation of covalent binding was performed by X-Ray co-crystallography. To confirm binding of rocbrutinib to WT and mutant BTK, we performed a NanoBRET assay against WT, C481S, T474I, and L528W BTK. To further measure the binding affinity of rocbrutinib and the currently available BTKi towards full-length WT and mutant BTK in HEK293T cells, we utilized a fluorescent probe cellular binding assay (FPCBA) (Yin et al., 2024). Using genetically modified TMD8 cells that express only C481S, T474I, or L528W mutated BTK, we determined the effect of rocbrutinib on cell-viability and BCR signaling. Primary CLL B-cells were isolated and treated with rocbrutinib for all experiments. BCR signaling alterations were assessed via immunoblot to observe changes in target protein phosphorylation. Changes in NFκB signaling were interrogated by RT-qPCR. In vivo studies were performed using Eμ-TCL1 and Eμ-MTCP1 mouse engraftment models.
Results
A crystal structure of BTK in complex with rocbrutinib at 1.7Å resolution showed rocbrutinib binds BTK in the ATP-binding site, forms a covalent bond to the C481 residue, and forms hydrogen bonds to M477, D539, and K430. In a NanoBRET assay, rocbrutinib demonstrated low nanomolar binding affinity towards the WT, C481S, T474I, and L528W BTK proteoforms with IC50 values of 4.7, 49.7, 13.1, and 80.4nM, respectively. This assay also showed rocbrutinib exhibits a long half-life when bound to WT and mutant BTK. Using FPCBA, rocbrutinib was the only BTKi—among ibrutinib, acalabrutinib, zanubrutinib, nemtabrutinib, and pirtobrutinib—to retain nanomolar potency against WT BTK as well as clinically relevant resistance mutations, including C481S, V416L, M437R, and L528W. In TMD8 cells, rocbrutinib maintained nanomolar GI50 towards WT, C481S, T474I, and L528W BTK. Rocbrutinib also inhibited BCR signaling regardless of BTK mutation status demonstrated by reducing production of CCL3 (WT: 98.8%, p< 0.0001; C481S: 99.1%, p< 0.0001; T474I: 98.9%, p< 0.0001; L528W: 99.6%, p< 0.0001) and CCL4 (WT: 97.3%, p< 0.0001; C481S: 96.3%, p< 0.0001; T474I: 97.3%, p< 0.0001; L528W: 99.3%, p< 0.0001) as well as inhibition BTK, PLCγ2, ERK, and AKT activation. Following two-hour drugging, 500nM rocbrutinib inhibited BCR signaling in primary CLL B-cells, demonstrated by reduced phosphorylation of BTK (98.9%, p< 0.0001), PLCγ2 (85.6%, p< 0.0001), ERK (59.3%, p=0.0029), and AKT (68.9%, p=0.0014). In patient samples, mRNA expression of NFκB pathway targets BCL2, BCL2L1, MCL1, BCL2A1, MYC, and CD40 were significantly decreased after 48-hours of treatment with 500nM rocbrutinib. Furthermore, we observed retained inhibition of BCR signaling in primary CLL B-cells harboring C481S via immunoblotting and cytokine production. Finally, to evaluate the in vivo efficacy of rocbrutinib, we evaluated its therapeutic impact in both the Eµ-TCL1 and Eµ-MTCP1 mouse models. We treated mice daily via oral gavage and found that 50 mg/kg of rocbrutinib significantly improved survival in the Eµ-TCL1 model when compared to vehicle (median 51 vs 44 days; p=0.0018) or ibrutinib at the same dose (median 51 vs 45 days; p=0.0098). Similarly, in the Eµ-MTCP1 model, rocbrutinib (50 mg/kg) markedly improved survival relative to vehicle (median 122 vs 62 days; p< 0.0001) or ibrutinib at the same dose (median 122 vs 96 days; p=0.0162).
Conclusion
Collectively, our findings demonstrate rocbrutinib is a potent and selective inhibitor of BTK with activity even in the presence of mutations that mediate resistance to cBTKi and ncBTKi. These data support the continued investigation of rocbrutinib, which is currently being studied in the phase 1 setting of CLL and NHL (NCT04775745 and NCT04993690).
Keywords : CLL, Relapsed/Refractory, BTK
Please indicate how this research was funded. : Leukemia and Lymphoma Society Career Grant
Please indicate the name of the funding organization.: Leukemia and Lymphoma Society