Authors
Vanthana Bharathi, MD, Kristofer Jennings, Jackie Broadway-Duren, Mahesh Swaminathan, MD, Stephanie Gabriella Zelaya, Dervy J Salcedo, Alessandra Ferrajoli, MD.
Background
Patients with CLL are at increased risk of infections and other cancers due to both disease-related immune dysfunction and treatment-related immunosuppression. While vaccination, routine cancer screening, and primary care engagement are well-established for the general population, their uptake in patients with CLL remains incompletely characterized, especially in the post-COVID-19 pandemic era.
Methods
We conducted a prospective, survey-based analysis of preventive health behaviors in patients with CLL from 2020 to 2025 to assess and improve adherence to preventive health recommendations. Each year, during in-person clinic visits, we administered a standardized health maintenance questionnaire that collected information on immunization history (influenza, pneumococcal, shingles, COVID-19), primary care visits, and age-appropriate cancer screenings (mammogram, Pap smear, PSA, colonoscopy, dermatologic skin exam). Due to COVID-19-related clinic disruptions, we paused the survey administration in 2021. To evaluate longitudinal adherence, we calculated cumulative uptake of influenza and COVID-19 vaccines among patients who completed multiple surveys. We used multivariable logistic regression to examine associations with demographic variables, adjusting for age, sex, race, ethnicity, and survey year. We reported odds ratios (OR) with 95% confidence intervals (CI).
Results
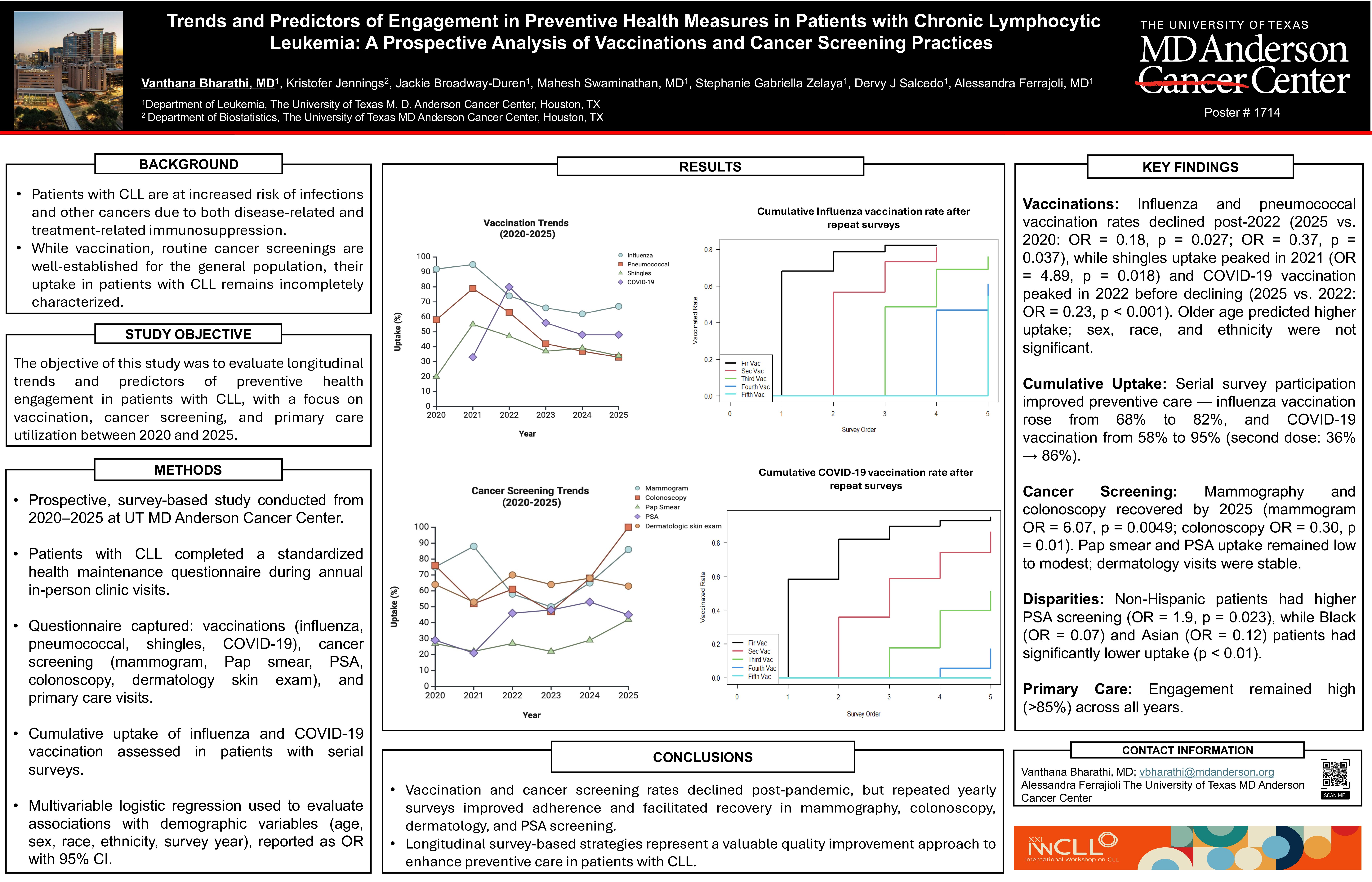
A total of 1,083 patients with CLL completed at least one survey. Yearly influenza vaccination rates declined from 92% in 2020 to 67% in 2025 (OR = 0.18, 95% CI: 0.02–1.51, p = 0.027). Pneumococcal vaccine uptake similarly dropped from 58% in 2020 to 33% in 2025 (OR = 0.37, 95% CI: 0.09–1.39, p = 0.037). Completion of at least one shingles vaccination was 20% in 2020, peaked at 55% in 2021 and declined to 34% by 2025. COVID-19 vaccination was recorded starting in 2021, was highest in 2022 at 80 % but fell to 48% in 2025 (OR 2025 vs 2022 = 0.23, 95% CI: 0.09–0.58, p = 1.9 x 10-5). Additionally, we identified older age as a consistent predictor of higher vaccine uptake across all vaccine categories, with a linear increase in odds per year of age. Sex, race, and ethnicity were not significant in multivariable models. Among patients with serial surveys, cumulative uptake of ≥2 doses were 81% for influenza and 74% for COVID-19 serving as indicators of sustained preventive engagement.
We evaluated sex and age-appropriate cancer screening rates in our patients. Mammography rates fell from 75% in 2020 to 50%, in 2023, then rebounded to 86% by 2025 (2025 vs. 2023 OR = 6.07, 95% CI: 1.04–35.4, p = 0.0049). Colonoscopy adherence declined from 76% in 2020 to 47% in 2023 (OR = 0.03, 95% CI: 0.07–1.12, p = 0.01), and then fully recovered to 100% by 2025 among a limited number of patients surveyed so far. Pap smear rates improved modestly from 27% in 2020 to 42% in 2025 (2025 vs. 2020: OR = 1.94, 95% CI: 0.19–18.9, p = 0.42). Prostate cancer screening rate followed a similar trend and increased from 29% in 2020 to 45% in 2025 (OR = 1.99, 95% CI: 0.38–10.5, p = 0.25). Ethnic disparities were noted in prostate cancer screenings: non-Hispanic patients had higher screening uptake (OR = 1.9, 95% CI: 1.1–3.4, p = 0.023). Racial disparities were also present—compared to White patients, Black patients had significantly lower screening odds (OR = 0.07, 95% CI: 0.029–0.184, p < 0.0001), as did Asian patients (OR = 0.12, 95% CI: 0.041–0.337, p < 0.0001). Skin cancer screening occurring at least once a year by a dermatologist was reported by 67% of patients and increased with age (OR/year = 1.035, 95% CI: 1.025–1.046, p = 2.6×10-11).
Primary care visit rates remained consistently high throughout the study period, with an overall engagement rate of 87%.
Conclusions
In this large, prospective CLL cohort, we observed a post-2022 decline in vaccination uptake across all vaccine types, with older age emerging as a consistent positive predictor. Serial survey participation was associated with higher cumulative adherence to influenza and COVID-19 vaccination. Cancer screening rates similarly declined during the pandemic but demonstrated partial recovery by 2025, particularly for mammography and colonoscopy. While primary care engagement remained high, racial and ethnic disparities persisted in specific preventive domains. These findings underscore the importance of sustained, targeted interventions to optimize preventive care in patients with CLL.
Keywords : vaccination, cancer screening, quality improvement
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: