Authors
Stephan Stilgenbauer, Lydia Scarfò, Ricardo D. Parrondo, Meghan C. Thompson, Anna Maria Frustaci, John N. Allan, Paolo Ghia, Irina Mocanu, Constantine S. Tam, Damien Roos-Weil, Judith Trotman, Inhye E. Ahn, Nicole Lamanna, Linlin Xu, Kunthel By, Shannon Fabre, Daniel Persky, Amit Agarwal, John F. Seymour.
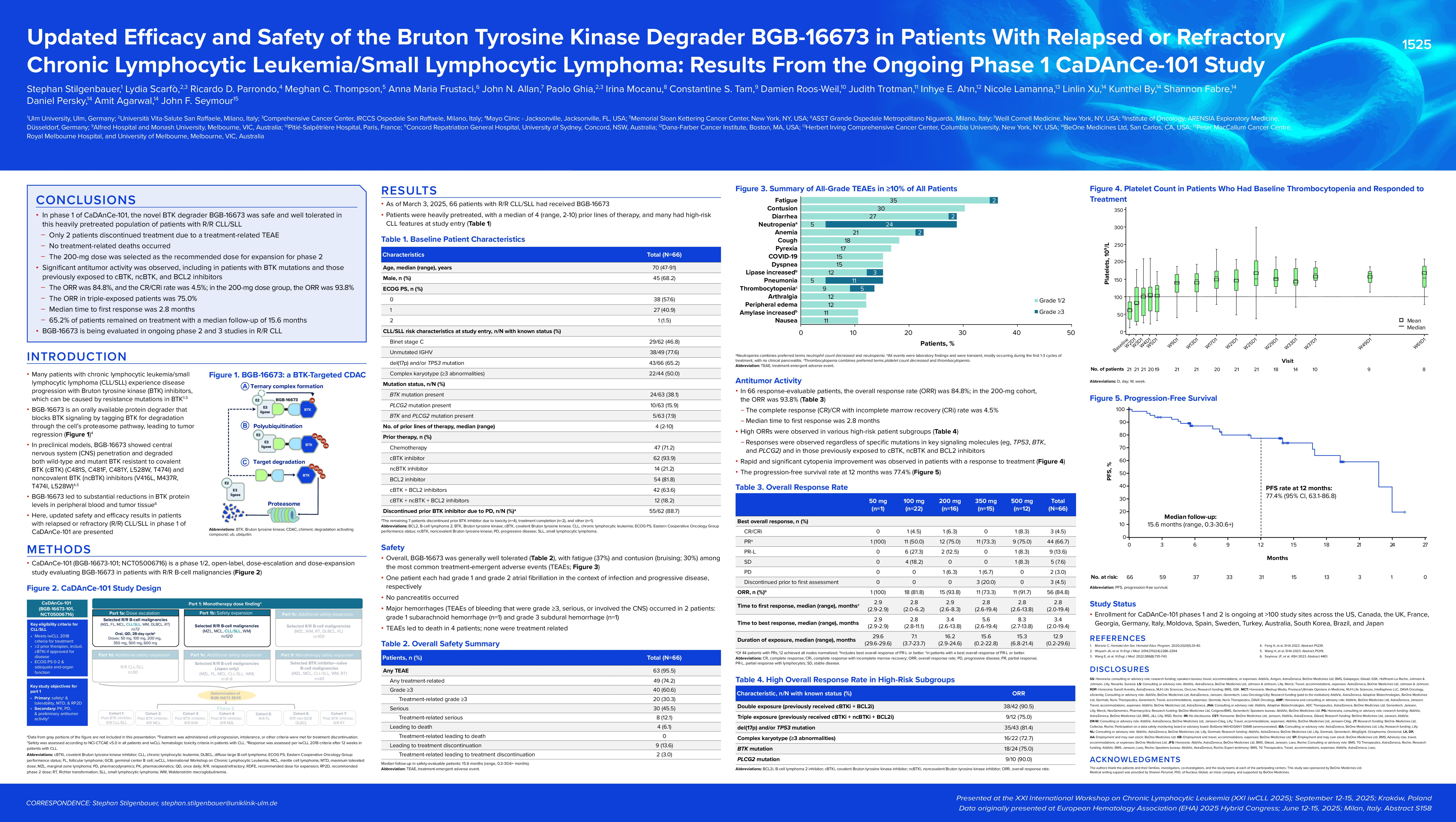
Background
Bruton tyrosine kinase (BTK) inhibitors are effective treatments for chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), but intolerance and/or acquired resistance due to BTK mutations can emerge. BGB-16673 is a protein degrader that blocks BTK signalling by tagging BTK for degradation through the cell’s proteasome pathway.
Aims
To describe updated phase 1 results for patients with relapsed/refractory (R/R) CLL/SLL in CaDAnCe-101 (BGB 16673-101; NCT05006716), a phase 1/2 open-label study.
Methods
Eligible patients must have confirmed R/R CLL/SLL (≥2 prior therapies), an Eastern Cooperative Oncology Group performance status of 0-2, and adequate organ function. In the US/EU/Australia, patients must have previously received a covalent BTK inhibitor (cBTKi). BGB-16673 was dosed once daily orally. Primary objectives were to assess safety/tolerability (CTCAE v5.0; iwCLL hematologic toxicity criteria) and establish the maximum tolerated dose and recommended dose for expansion. A secondary objective was to assess overall response rate (ORR) (iwCLL 2018 criteria with partial response with lymphocytosis [PR-L] modification; 2014 Lugano criteria for SLL).
Results
As of December 17, 2024, 66 patients with CLL/SLL were enrolled and treated (50 mg, n=1; 100 mg, n=22; 200 mg, n=16; 350 mg, n=15; 500 mg, n=12). Median age was 70 (range 47 91) years; the median number of prior therapies was 4 (range, 2-10), including prior cBTKis (n=61; 92.4%), BCL2 inhibitors (BCL2is; n=54; 81.8%), and noncovalent BTKis (ncBTKis; n=14;21.2%). In total, 65.2% (43/66) of patients had del(17p) and/or TP53 mutation and 79.6% (39/49) had unmutated IGHV. Median follow-up was 13.1 (range, 0.3-29.9) months.
Overall, 92.4% of patients had any-grade treatment-emergent adverse events (TEAEs; grade ≥3, 51.5%); those in ≥30% of patients were fatigue (36.4%; grade ≥3, 1.5%) and contusion/bruising (30.3%; no grade ≥3). Grade ≥3 TEAEs in ≥10% of patients were neutropenia/neutrophil count decreased (21.2%) and pneumonia (12.1%). Atrial fibrillation (grade 1 in the context of bacterial pneumonia) and febrile neutropenia (in the context of COVID-19 pneumonia and norovirus diarrhea) occurred in 1 pt (1.5%) each. Hypertension (n=2, both grade 3) and major hemorrhage occurred in 2 patients each (3.0%, grade 1 subarachnoid hemorrhage resolved; grade 3 subdural hemorrhage outcome unknown). Six patients (9.1%) had a TEAE leading to dose reduction. Four patients had TEAEs that led to death (pneumonia in the context of disease progression, septic shock, bronchopulmonary and cerebral aspergillosis, and acute respiratory failure; n=1 each); no deaths were deemed related to BGB-16673.
In 66 response-evaluable patients, ORR (PR-L or better) was 80.3% (n=53), and complete response (CR)/CR with incomplete recovery (CRi) rate was 3.0% (n=2). At 200 mg, ORR was 93.8% (15/16), including 1 CR. Median time to first response was 2.8 (range, 2.0-10.9) months. Thirty-three patients (50.0%) remained on treatment for ≥12 months; 38 patients had ongoing responses. Responses deepened over time: of 19 patients with initial PR-L, 10 transitioned to partial response (PR) and 1 to CR; of 15 patients with initial stable disease, 1 transitioned to PR-L, 5 to PR, and 1 to CRi. Responses were seen at the lowest dose (50 mg, 1/1); in patients previously treated with a cBTKi (49/61; 80.3%) or ncBTKi (10/14; 71.4%) and with double- (cBTKi and BCL2i; 36/41; 87.8%) and triple-exposure (cBTKi, BCL2i, ncBTKi; 9/12; 75.0%); and in patients with (17/24; 70.8%) and without (33/39; 84.6%) BTK mutations, and with del(17p) and/or TP53 mutation (33/43; 76.7%). Median progression-free survival was not reached.
Summary/Conclusion
Data from this ongoing study demonstrate that the novel BTK degrader BGB-16673 has a tolerable safety profile and shows robust and deepening responses in patients with heavily pretreated R/R CLL/SLL, including those with prior BTKi treatment and BTKi mutations.
Keywords : chronic lymphocytic leukemia, dose escalation, Phase 1
Please indicate how this research was funded.:
Please indicate the name of the funding organization. : BeOne Medicines Ltd