Authors
Eun Sang Yu, Soyean Kwon,Sung-Soo Park, Ja Min Byun, Youngil Koh,Ki-Seong Eom, Chul Won Choi.
Background
Since the FDA approval of Bruton’s tyrosine kinase inhibitor (BTK inhibitor) ibrutinib in 2012, the treatment landscape for chronic lymphocytic leukemia (CLL) and small lymphocytic leukemia (SLL) has undergone transformative changes. However, the disease remains incurable, posing a long-term challenge. In Korea, the younger median age at diagnosis and higher annual percentage change (4.17% in Korea vs. 0.68% in United states during 1999 to 2010) suggest a growing prevalence and healthcare burden. This study aims to provide updated epidemiologic data to guide care planning and support innovative therapeutic approaches.
Methods
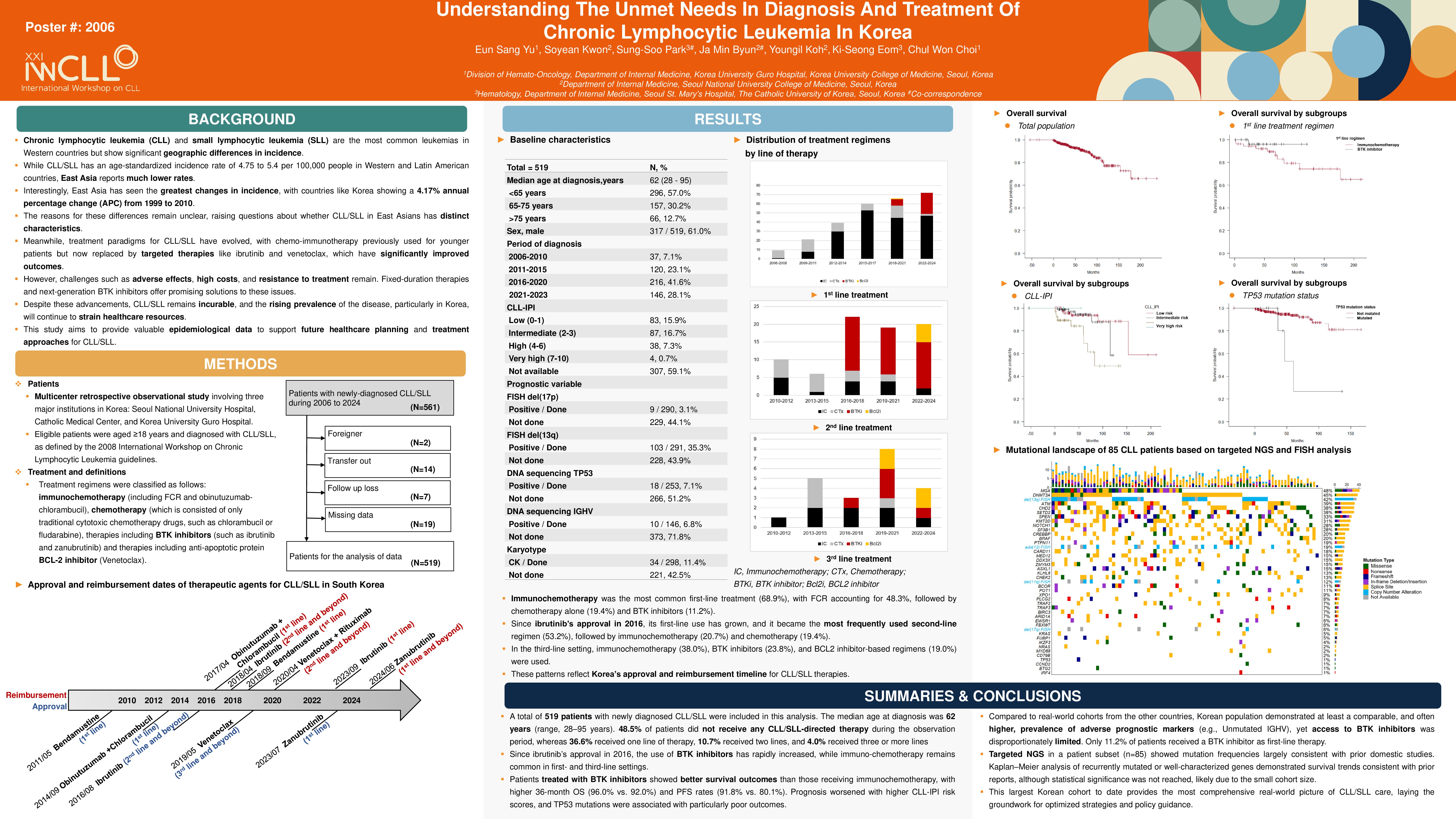
This multicenter retrospective study included 519 patients diagnosed with CLL/SLL between 2006 and 2024 across three major Korean institutions. Their medical records were reviewed and analyzed for demographics, baseline disease characteristics, details of treatment, treatment outcomes and survival. When available, results from cytogenetic and molecular genetics data were collected. Treatment regimens were classified as follows: immunochemotherapy (including fludarabine- cyclophosphamide-rituximab and obinutuzumab-chlorambucil), chemotherapy (which is consisted of only traditional cytotoxic chemotherapy drugs, such as chlorambucil or fludarabine), BTK inhibitors and BCL-2 inhibitor.
Results
The median follow-up period was 45.3 months. Of the 519 patients (median age at diagnosis 62 years;61% male), cytogenetic data, including FISH and karyotyping, were available for nearly half (55.9 – 57.5%) of the study population. TP53 mutations were detected in 7.1% (18/253), and unmutated IGHV was found in 93.1% (136/146) of patients. International Prognostic Index for Chronic Lymphocytic Leukemia (CLL-IPI) scores could be calculated for 40.9% of the cohort, among whom 15.9% and 16.7% were classified as low- and intermediate-risk, respectively, while high-risk and very high-risk categories comprised 7.3% and 0.7% of patients. In a cohort of 267 patients who received first-line treatment, 68.9% (n=184/267) underwent immunochemotherapy, 19.4% (n=52/267) received cytotoxic chemotherapy, and 11.2% (n=30/267) were treated with BTK inhibitor. BTK inhibitor use has steadily increased since 2016, following ibrutinib’s approval for CLL/SLL treatment in Korea. Subgroup analyses of showed that higher CLL-IPI scores correlated with poorer overall and progression-free survival. Compared to the low-risk group, the high- and very high-risk group had a significantly increased risk of death (HR 5.16, 95% CI 1.71-15.56, p = 0.004) and progression (HR 7.49, 95% CI 2.48-22.64, p=0.0003). Regarding treatment modality, individuals receiving BTK inhibitor demonstrated more favorable outcomes compared to those treated with immunochemotherapy. The 36-month Overall survival (OS) and Progression-free survival (PFS) rate were 96.0% vs 91.3% and 91.8% vs 79.7%, respectively, favoring the BTK inhibitor-based therapy.
Discussion
Although patients with CLL/SLL in Korea are diagnosed at a younger age than those in Western countries, first-line treatment outcomes are not notably superior. This may reflect differences in therapeutic approaches, with immunochemotherapy remains the predominant regimen in Korea, whereas BTK inhibitors are more commonly used in Western populations (11.2% in Korea vs 45.0% in United states (Clin Lymphoma Myeloma Leuk. 2024;24(9):e301–e313.) and 31.2% in Spain (Clin Lymphoma Myeloma Leuk. 2021;21(12):e985–e999.). While acknowledging the inherent limitations of cross-national comparisons — including disparities in healthcare infrastructure and treatment accessibility — similar trends were observed within our cohort. Patients aged >= 65 years received BTK inhibitor more frequently than younger patients (12.8%, 15/117 vs 10.0%, 15/150) and were less often treated with immunochemotherapy (64.9%, 76/117 vs 72.0%, 108/150). Despite their older age and likely comorbidity burden, overall response rates were comparable between these two groups (Overall response rate [ORR] 82.9% [Complete response (CR) 51;Partial response (PR) 46] vs 88.6% [CR 93;PR 40]. Although these findings are subject to potential confounding, they support the feasibility and potential clinical benefit of broader BTK inhibitor use in Korea, where access remains limited by reimbursement policies. Additionally, despite the demonstrated prognostic value of the CLL-IPI, its use remains limited in Korea due to the low rate of genetic testing. Beyond CLL-IPI, comprehensive genetic testing plays a critical role in modern CLL/SLL management. The integration of molecular and response-based biomarkers is redefining not only risk stratification, but also response assessment and treatment decision-making, including considerations for therapy discontinuation. Optimizing CLL/SLL management thus requires not only broadening access to effective agents but also implementing precision medicine tools to match treatment intensity with disease risk and response.
Keywords : Chronic lymphocytic leukemia, Small lymphocytic leukemia, Real-world data
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: