Authors
Tingyu Wang, Yuting Yan, Zengjun Li, HuiWang, Ying Sun, Xiantao Liu, Rui Lyu, Wenjie Xiong, Gang An, Wei Liu, Yan Xu, Shuhui Deng, Qi Wang, Chenxing Du, Liang Huang, Dehui Zou, Yaozhong Zhao, Lugui Qiu, Shuhua Yi.
Background
BTK inhibitors, such as ibrutinib, have propelled chronic lymphocytic leukemia (CLL) into the era of targeted therapy. Nevertheless, continuous treatment with these agents not only leads to a progressive increase in resistance but also escalates treatment costs. On the other hand, the FCR regimen, consisting of fludarabine, cyclophosphamide, and rituximab, holds curative potential for CLL. However, its clinical application is significantly hampered by severe toxicity and long-term risks. To address these challenges, we developed the HAMBURGER regimen, a novel time-limited, alternating treatment approach combining ibrutinib with three cycles of FCR. This regimen aims to achieve deep remissions in CLL patients while enhancing tolerability and establishing a fixed treatment duration.
Methods
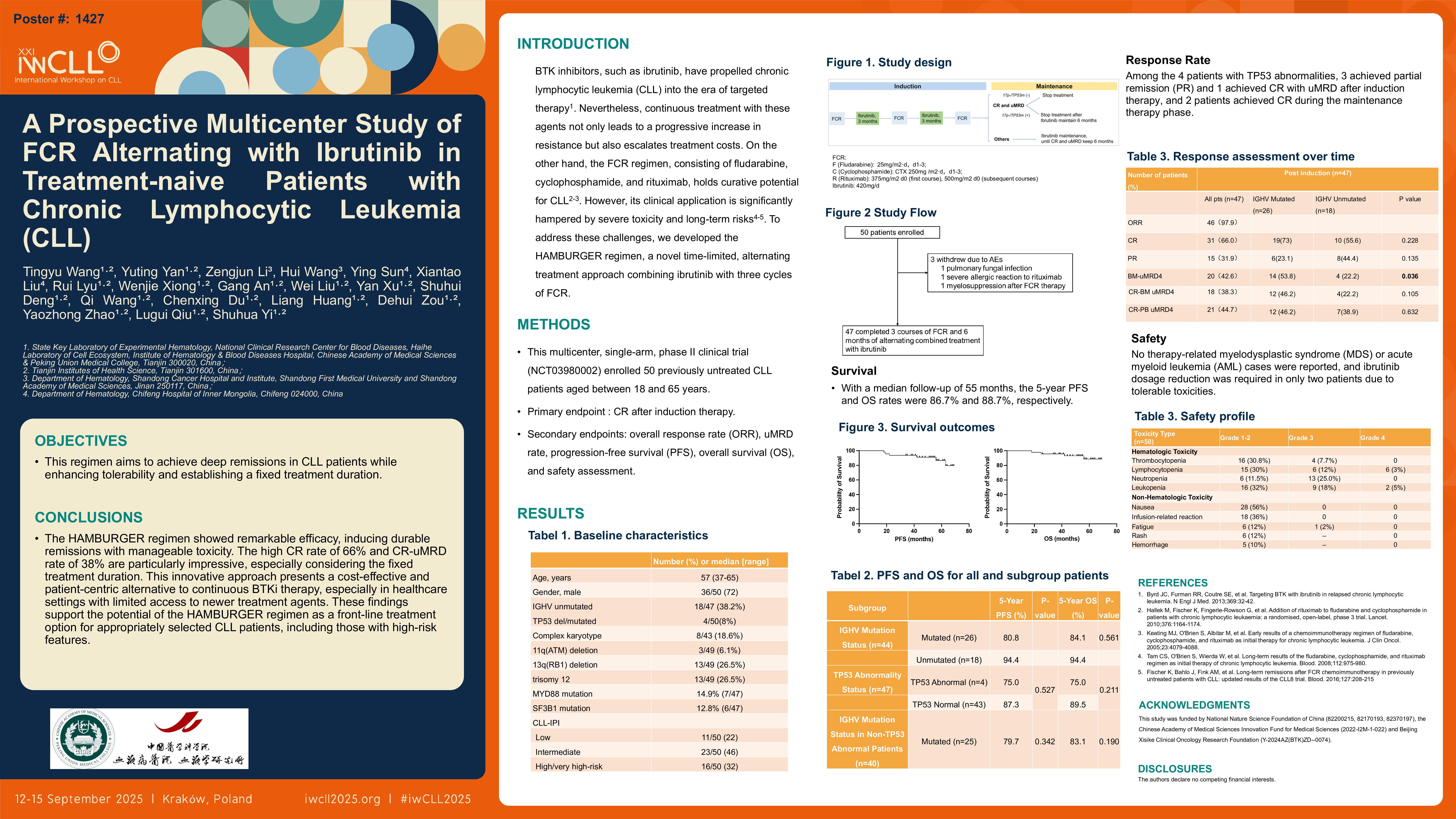
This multicenter, single-arm, phase II clinical trial (NCT03980002) enrolled 50 previously untreated CLL patients aged between 18 and 65 years. The treatment protocol involved the induction therapy: one cycle (lasting one month) of FCR, followed by three months of ibrutinib monotherapy at a dosage of 420 mg per day, then two alternating cycles of FCR and ibrutinib were given and the maintenance therapy with ibrutinib monotherapy after induction.
After the completion of induction therapy, the treatment discontinuation strategy was based on the achievement of complete remission (CR) with undetectable minimal residual disease (uMRD) and TP53 status: patients without TP53 deletion or mutation could discontinue treatment; those with TP53 deletion or mutation continued maintenance therapy for six months before stopping; all other patients continued single-agent ibrutinib maintenance until they achieved CR with uMRD, followed by an additional six months of treatment. The primary endpoint of this study was the achievement of CR after induction therapy. Secondary endpoints included overall response rate (ORR), uMRD rate, progression-free survival (PFS), overall survival (OS), and safety assessment.
Results
Among the 50 enrolled patients (with a median age of 57 years and 72% being male), 47 completed the induction therapy. The overall response rate (ORR) was 97.9% (46/47), with 66.0% (31/47) of patients achieving CR. Notably, 38.3% (18/47) of patients achieved CR with undetectable MRD in both bone marrow and peripheral blood. The bone marrow uMRD rate after induction therapy was 42.6% (20/47). Patients with immunoglobulin heavy chain variable region (IGHV)-mutated status demonstrated a higher bone marrow uMRD rate (53.8% vs. 22.2%, p=0.036). Among the 4 patients with TP53 abnormalities, 3 achieved partial remission (PR) and 1 achieved CR with uMRD after induction therapy, and 2 patients achieved CR during the maintenance therapy phase.
With a median follow-up of 55 months, the 5-year PFS and OS rates were 86.7% and 88.7%, respectively. In IGHV-unmutated patients, the 5-year PFS and OS were both 94.4%, compared with 80.8% and 84.1% in IGHV-mutated patients (PFS: p=0.666; OS: p=0.561). For patients with TP53 abnormalities, the 5-year PFS and OS were 75.0%, which were lower than those in patients without TP53 abnormalities (PFS 87.3%, OS 89.5%), although the differences did not reach statistical significance (PFS: p=0.527; OS: p=0.211). Among the 28 patients who received ibrutinib maintenance therapy, five patients transitioned from PR to CR. Fourteen patients discontinued ibrutinib, including nine who did so voluntarily, and only one patient experienced relapse and successfully resumed ibrutinib treatment.
Safety was evaluated in all 50 enrolled patients. Hematologic toxicities were common, with leukopenia observed in 24 (48.0%) patients, thrombocytopenia in 20 (40.0%), and lymphocytopenia in 27 (54.0%). Grade 3/4 neutropenia occurred in 26% of patients. Non-hematologic adverse events (AEs) were predominantly Grade 1–2, including nausea (56%) and infusion reactions (36%). No therapy-related myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML) cases were reported, and ibrutinib dosage reduction was required in only two patients due to tolerable toxicities.
Conclusion
The HAMBURGER regimen showed remarkable efficacy, inducing durable remissions with manageable toxicity. The high CR rate of 66% and CR-uMRD rate of 38% are particularly impressive, especially considering the fixed treatment duration. This innovative approach presents a cost-effective and patient-centric alternative to continuous BTKi therapy, especially in healthcare settings with limited access to newer treatment agents. The MRD-guided treatment discontinuation strategy further enhances the long-term benefits and practicality of this regimen. These findings support the potential of the HAMBURGER regimen as a front-line treatment option for appropriately selected CLL patients, including those with high-risk features.
Keywords : CLL, time limited regimen, u MRD
Please indicate how this research was funded.: This work was supported by grants from the National Nature Science Foundation of China (82200215, 82170193, 82170194, 82370197), the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2022-I2M-1-022) and Beijing Xisike Clinical Oncology Research Foundation (Y-2024AZ(BTK)ZD–0074).
Please indicate the name of the funding organization. : National Nature Science Foundation of China (82200215, 82170193, 82170194, 82370197), the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2022-I2M-1-022) and Beijing Xisike Clinical Oncology Research Foundation (Y-2024AZ(BTK)ZD–0074)