Authors
Temitope Erinfolami, Amelia Fisher, Indrani Karpha, Yeong Lim, Nurunnahar Akter, Toyyib Abdulkareem, Brogan Johnston, Catrin Tudur Smith, Hilary Lindsay, Shaun Bowden, Debbie Yates, Lelia Duley, David Allsup, Hanhua Liu, Andrew Pettitt, Nagesh Kalakonda, Mark Bishton, Nicolas Martinez-Calle.
Background-Aim
Population-based datasets are essential for understanding epidemiology and evaluating the impact of changes in therapeutic paradigms for conditions such as chronic lymphocytic leukaemia (CLL). UNCOVER is a blood cancer health data research programme that utilises routinely collected NHS data provided by the National Disease Registration Service (NDRS). The data is a quality-assured collation from multiple sources and includes unselected patients diagnosed with haematological malignancies in England from 2014 to 2021, along with patient-level survival and treatment data. The present study used this data to profile the recent epidemiology of CL L in England.
Methods and Cohort Description
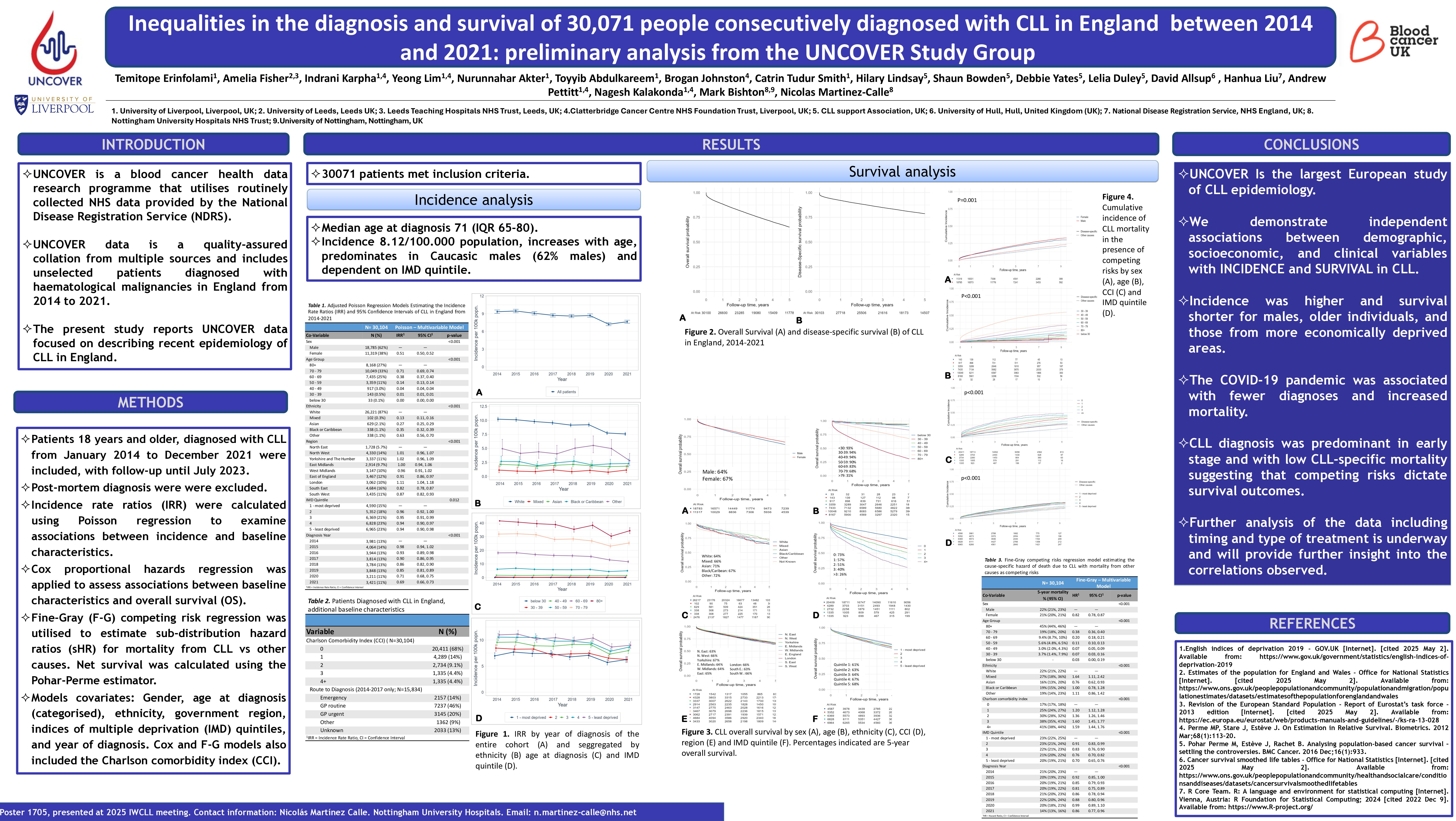
Information was available on 30,071 patients aged ≥18 who were diagnosed with CLL from January 2014 to December 2021 with follow-up until July 2023. Diagnoses made by death certificate only were excluded. Incidence rate ratios (IRR) were calculated using Poisson regression to examine associations between incidence and baseline characteristics. Cox proportional hazards regression was applied to assess associations between baseline characteristics and overall survival (OS). Fine-Gray (F-G) competing risk regression was utilised to estimate sub-distribution hazard ratios (sHR) for mortality from blood cancer vs other causes. Net survival was calculated using the Pohar-Perme estimator. Models included gender, age at diagnosis (categorised), ethnicity, government region, indices of multiple deprivation (IMD) quintiles, and year of diagnosis. The Cox and F-G models also included the Charlson comorbidity index (CCI).
Incidence analysis
The age-standardised incidence of CLL peaked at 8.12 per 100,000 population in 2015 and dropped to 5.94 per 100,000 in 2020. Males accounted for 62% of cases, median age at diagnosis of 72 years (IQR: 65–80). Females were 49% less likely to develop CLL compared to males [IRR = 0.51; 95% CI: 0.50, 0.52]. Predominant ethnicity was white (87%), and most (68%) had a CCI of 0. Among years with data available for route of diagnosis, most (54%) were referred via primary care, while a minority (10.6%) were identified via emergency presentation . Incidence rates for the least deprived areas were lower than for the most deprived areas with an IRR of 0.94 (95% CI: 0.91, 0.98). Compared to 2014, the rates of CLL diagnoses were lowest in 2020 [IRR = 0.72; 95% CI: 0.69, 0.76] and 2021 [IRR = 0.70; 95% CI: 0.67, 0.74] coinciding with the COVID pandemic. All examined factors (age, gender, ethnicity, region, deprivation quintile and year of diagnosis were independently associated (P < 0.01) with CLL incidence in multivariable analysis. Analysis by government region showed lower incidence outside Greater London, with the Southeast accounting for the lowest rate [IRR = 0.70; 95% CI: 0.67, 0.74].
Survival Analysis
Median follow-up time was 49.1 months. 37.5% of patients died with OS rates at 1, 3 and 5 years of 88%, 76%, and 65%, respectively, while the corresponding net survival rates were 92%, 85%, and 79%, suggesting that patients become increasingly susceptible to non-CLL causes of mortality as they survive longer. Cox regression showed that the risk of all-cause mortality was 19% lower in females compared to males [HR = 0.81; 95% CI: 0.78, 0.84] and 31% lower among individuals from the least deprived areas compared to their counterparts in the most deprived neighbourhoods [HR = 0.69; 95% CI: 0.65, 0.74] . The hazard ratio for all-cause mortality was highest for patients diagnosed in 2020 [HR = 1.21; 95% CI: 1.12, 1.32] compared to 2014. The F-G model for competing risk of survival showed year of diagnosis, age, ethnicity, region and CCI were independently associated with OS and competing risk survival, with no significant increase in the sHR when compared to the Cox model, suggesting a low CLL-related mortality in this cohort .
Conclusions
UNCOVER has provided the largest European study of CLL epidemiology and demonstrated to date, with clear associations with demographic, socioeconomic, and clinical variables. Incidence was higher and survival shorter for males, older individuals, and those from more deprived areas. The COVID-19 pandemic was associated with fewer diagnoses and increased mortality. Most patients were diagnosed early, with low CLL-specific mortality suggesting that competing survival risks play a significant role in long-term outcomes. Further analysis of the data including timing and type of treatment is underway and will provide further insight into the correlations observed in this initial analysis.
Keywords : Population-based, real world, CLL, inequalities, incidence, net survival.
Please indicate how this research was funded. :
Please indicate the name of the funding organization.: Cancer Research UK, Grant Ref. 23010