Authors
Krzysztof Jamroziak, Elzbieta IskierkaJazdzewska, Tadeusz Robak, Klaudia Zielonka, Sebastian Giebel, Kamil Wisniewski, Joanna Drozd Sokolowska, Justyna Rybka, Weronika Piszczek, Monika Joks, Anna Dabrowska Iwanicka, Andrzej Mital, Paweł Steckiewicz, Ewa Lech Maranda, Marcin Jasinski, Marcin Rymko, Dawid Marciniak, Tomasz Wrobel, Lidia Gil, Joanna Romejko, Jarosinska, Dorota Kruk Kwapisz, Agnieszka Chudy, Marcin Machnicki, Krzysztof Giannopoulos, Tomasz Stoklosa, Bartosz Pula.
Introduction
Fixed-duration regimens combining a selective BCL-2 inhibitor, venetoclax, with an anti-CD20 antibody (rituximab or obinutuzumab) are the mainstay of current management of chronic lymphocytic leukemia (CLL). However, it is unknown whether the same duration of treatment is optimal for all patients. Clinical trials have shown that achieving undetectable measurable residual disease (MRD) with venetoclax-based regimens is associated with superior long-term outcomes in CLL. It can be therefore hypothesized that adjusting the duration of therapy to MRD status may provide an optimal balance between treatment activity and toxicity.
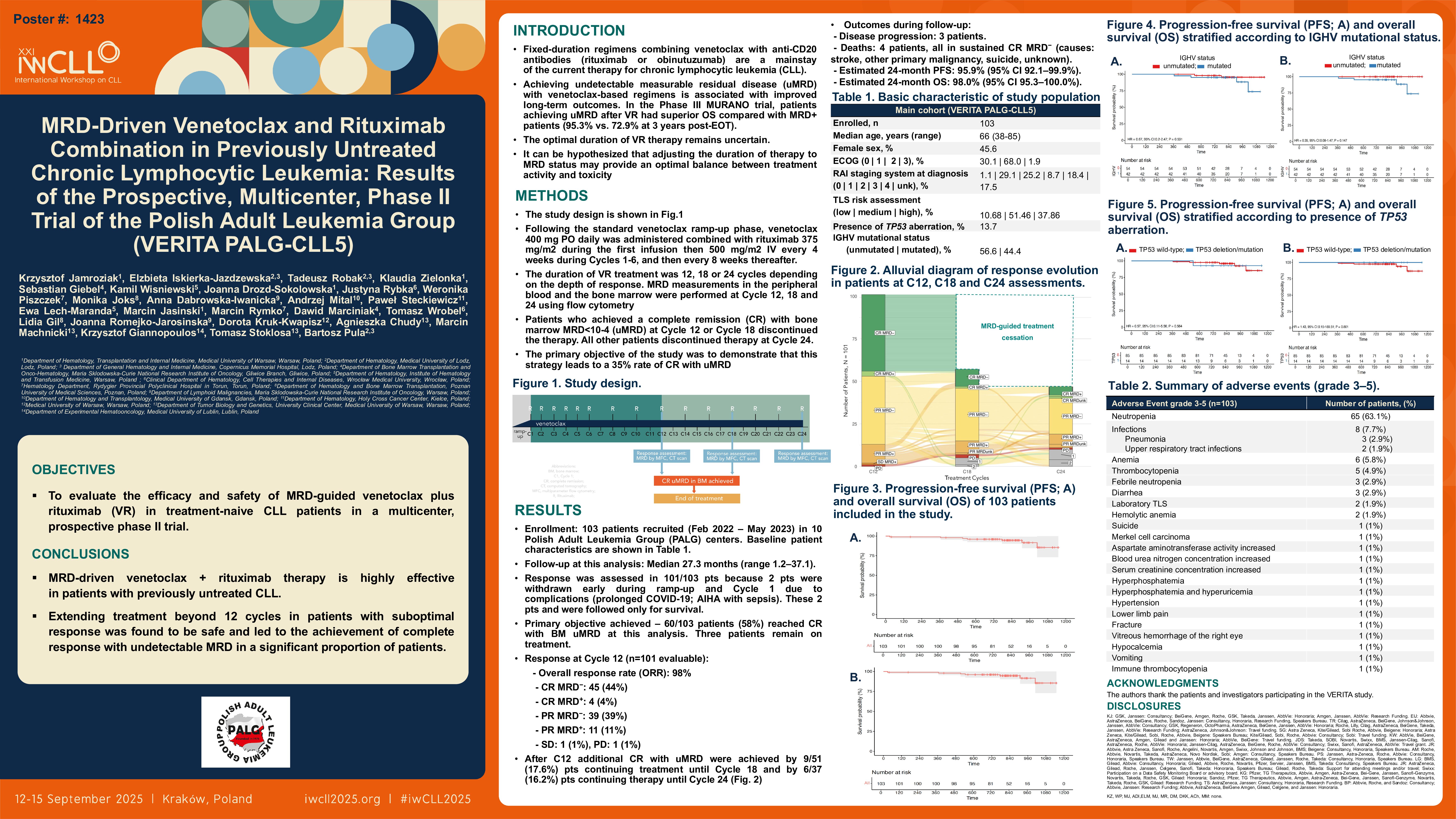
Methods
This prospective, multicenter, phase II study aimed to assess the efficacy and safety of MRD-driven combination of venetoclax and rituximab (VR) in treatment-naïve CLL. Following the standard venetoclax ramp-up phase, patients received venetoclax 400 mg orally once daily, combined with rituximab 375 mg/m2 during the first infusion, then 500 mg/m2 intravenously every 4 weeks during Cycles 1-6, and every 8 weeks thereafter. Treatment duration was determined based on depth of response, with VR administered for 12, 18, or up to 24 cycles. For patients who achieved a complete remission (CR) with bone marrow MRD < 10-4 (MRD-) by flow cytometry at the response assessments at Cycle 12 or Cycle 18, therapy was discontinued. The primary objective of the study was to demonstrate that this strategy leads to a 35% CR MRD- rate. Here, we present the results of a preplanned interim analysis performed after all study participants had responses assessed at Cycle 12.
Results
Between February 2022 and May 2023, all planned 103 patients were recruited in 10 Polish Adult Leukemia Group centers. The patients’ median age was 66 years (range 38-85), and 56 (54%) of them were male. Del17p or TP53 mutation were present in 13 (13%) patients. Unmutated IGHV was found in 53 (51%) patients, mutated IGHV in 41 (40%), while IGHV status was undetermined in 9 patients. Tumor lysis syndrome (TLS) risk was high in 38% and medium in 51% of patients. The median study follow-up time was 27.3 months (1.2 – 37.1). Response to treatment was assessed in 101 patients, as two were withdrawn early (ramp-up and Cycle 1) due to complications (prolonged COVID-19 and autoimmune hemolytic anemia (AIHA) with sepsis) and followed only for survival. The study met its primary endpoint with CR with bone marrow MRD- achieved by 60 (58%) study participants, while three patients continued the therapy. At the assessment at Cycle 12, the overall response rate (ORR) was 98%, including 45 (44%) CR MRD-, 4 (4%) CR MRD+, 39 (39%) partial remission (PR) MRD-, 11 (11%) PR MRD+, 1 (1%) stable disease and 1 (1%) progressive disease. Notably, 9 (17.6%) patients who continued therapy to Cycle 18, and additional 6 (16.2%) patients who continued therapy to Cycle 24, achieved CR MRD- response. During the follow-up period, three patients experienced disease progression. Four deaths were recorded, all in patients maintaining CR MRD- response (reason of death: stroke, other primary malignancy, suicide, and one unknown). The estimated 24-month progression-free survival (PFS) was 95.9% (95% CI 92.1 – 99.9%), and overall survival (OS) was 98.0% (95% CI 95.3 – 100.0%).
Treatment was generally well tolerated. Hematological toxicity was the most prominent, with neutropenia of all grades (G) comprising 38% of adverse events (AEs). Grade 3/4 AEs were noted in 72 (69.9%) patients including G3/4 neutropenia observed in 66 (64.1%) study participants. However, G 3/4 infections were reported only in 7 (6.8%) patients. Other AEs of interest included 5 cases of laboratory TLS, 3 AIHA, and 2 second primary malignancies.
Conclusions
The results of the VERITA PALG-CLL5 study indicate high efficacy of MRD-driven venetoclax plus rituximab combination in treatment-naïve CLL. Extending treatment beyond 12 cycles in patients with suboptimal response was safe and led to the achievement of CR MRD- response in a significant proportion of patients.
Keywords : chronic lymphocytic leukemia; venetoclax; measurable residual disease
Please indicate how this research was funded.: The study has received financial support from pharmaceutical company.
Please indicate the name of the funding organization. : AbbVie Inc.