Authors
Lindsey E. Roeker, M.D, Kari G. Rabe, M.S, Paul J. Hampel, M.D, Yucai Wang, M.D. Ph.D, Eli Muchtar, M.D, Saad J. Kenderian, M.B, Ch.B, Mazie Tsang, M.D, Jose F. Leis, M.D. Ph.D, Talal Hilal, M.D, Ricardo D. Parrondo, M.D, Min Shi, M.D. Ph.D, Curtis A. Hanson, M.D, Cinthya J. Zepeda Mendoza, Ph.D, Amber B. Koehler, P.A.-C., M.S, Amy L. Behnken, APRN, C.N.P, M.S, Catherine C. Wagner, APRN, C.N.P, D.N.P, Monica I. Aasum, R.N, Kersten R. Thomas, R.N, Maria A. Nuli, R.N, Rachel J. Bailen, Pharm.D., R.Ph., BCPS, Susan M. Schwager, B.S, Susan L. Slager, Ph.D, Neil E. Kay, M.D, Sameer A. Parikh, M.B.B.S.
Introduction
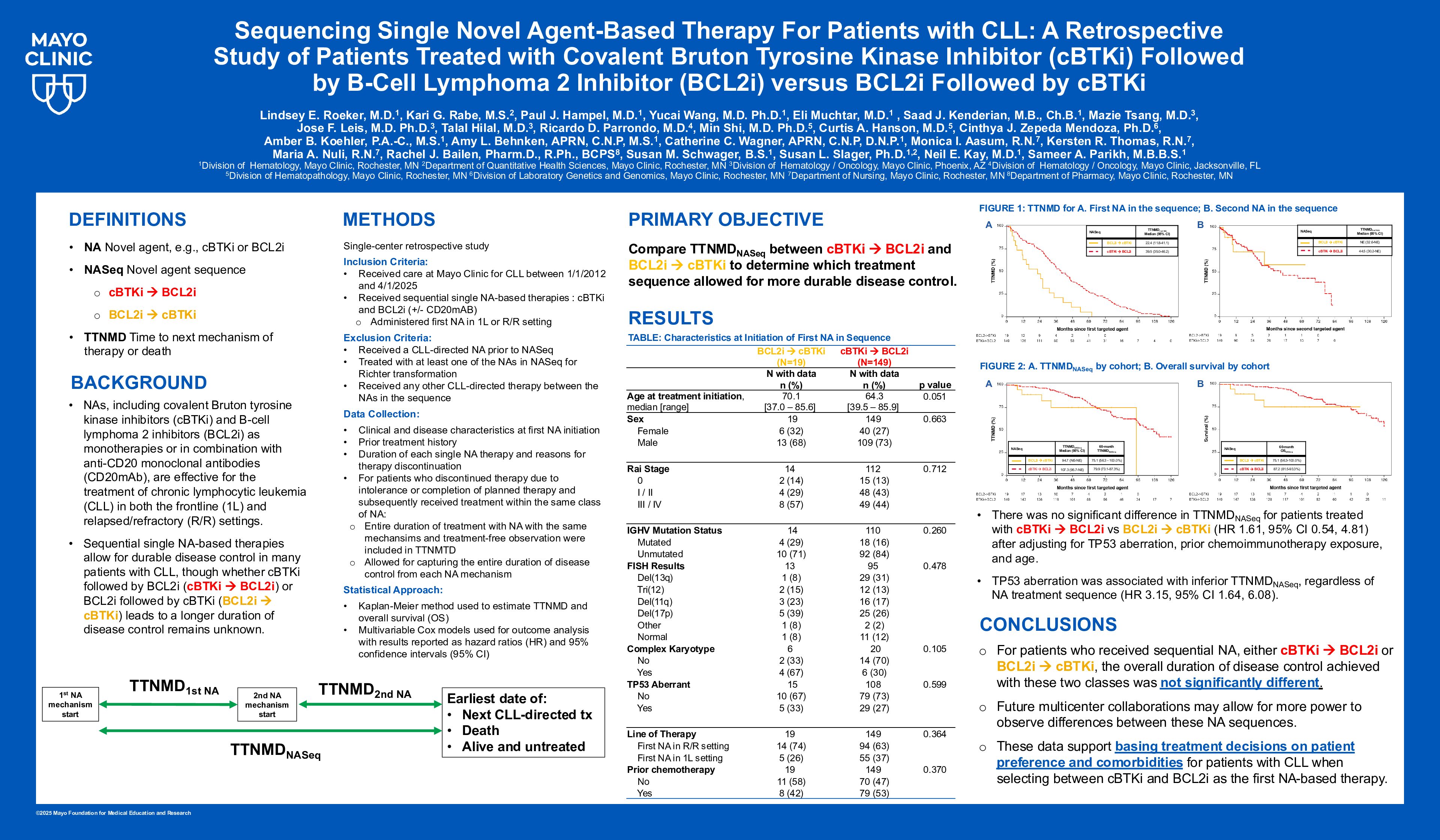
Novel agents, including covalent Bruton tyrosine kinase inhibitors (cBTKi) and B-cell lymphoma 2 inhibitors (BCL2i) as monotherapies or in combination with anti-CD20 monoclonal antibodies (CD20mAb), are effective for the treatment of chronic lymphocytic leukemia (CLL) in both the frontline (1L) and relapsed/refractory (R/R) settings. Sequential single novel agent-based therapies allow for durable disease control in many patients with CLL, though whether cBTKi followed by BCL2i (cBTKi->BCL2i) or BCL2i followed by cBTKi (BCL2i->cBTKi) leads to a longer duration of disease control remains unknown.
Methods
In this single-center retrospective study, we examined patients seen at Mayo Clinic for CLL between 1/1/2012 and 4/1/2025 who had received cBTKi- or BCL2i-based therapy during their disease course. We then identified patients who received sequential single novel agent-based therapies (monotherapy or in combination with CD20mAb; the first novel agent in the sequence could be used in either the 1L or R/R setting) to establish two cohorts: cBTKi->BCL2i and BCL2i->cBTKi. Patients were excluded if they had received (1) a CLL-directed novel agent prior to the sequence of interest, (2) novel agent-based treatment under study for Richter transformation, or (3) any other CLL-directed therapy between the treatments under study.
We examined baseline clinical and disease characteristics at the time of initiation of the first novel agent, as well as prior treatment history. Duration of each single novel agent therapy and reasons for therapy discontinuation were recorded. For patients who discontinued therapy due to intolerance or completion of planned therapy and subsequently received treatment within the same class of novel agent, the entire duration of treatment and treatment-free observation was included in duration of therapy. This method allowed for capturing the entire duration of disease control from each novel agent mechanism.
The Kaplan-Meier method was used to estimate time to next mechanism of therapy or death (TTNMD) and overall survival (OS). Cox models were used for outcome analysis. TTNMD[cBTKi] was defined as time from initiation of cBTKi therapy to initiation of the BCL2i, alternate CLL-directed therapy following BCL2i->cBTKi, or death, whichever occurred first. TTNMD[BCL2i] was defined as time from initiation of BCL2i therapy to initiation of cBTKi, alternate CLL-directed therapy following cBTKi->BCL2i, or death, whichever occurred first. TTNMD[cBTKi+BCL2i] encompassed TTNMD for the combination of both agents, regardless of sequence. The primary objective was to compare TTNMD[cBTKi+BCL2i] between the cohorts to determine which treatment sequence allowed for more durable disease control.
Results
149 patients received cBTKi->BCL2i, and 19 received BCL2i->cBTKi. At initiation of the first novel agent, median age was 65 years (range 58-73), 73% were male, Rai stage was III/IV in 45%, 82% (102/124) had unmutated IGHV, and 28% (34/123) had TP53 aberration; characteristics were not significantly different between the cohorts, though patients who received cBTKi->BCL2i tended to be younger (median age 64 vs 70 years, p=0.051) and had a lower proportion of TP53 aberration (25% vs 46%, p=0.16). The majority received the first novel agent in the R/R setting (63% of cBTKi->BCL2i and 74% of BCL2i->cBTKi); 36% received the first novel agent in the sequence in the 1L setting (37% cBTKi->BCL2i and 26% BCL2i->cBTKi). Fifty-two percent received chemoimmunotherapy prior to the novel agent-based sequences (53% cBTKi->BCL2i and 42% BCL2i->cBTKi).
Median TTNMD[cBTKi+BCL2i] was 107 months for cBTKi->BCL2i and 95 months for BCL2i->cBTKi (p=0.18). There was no significant difference in TTNMD[cBTKi+BCL2i] for patients treated with cBTKi->BCL2i vs BCL2i->cBTKi (HR 1.61, 95% CI 0.54, 4.81) after adjusting for TP53 aberration, prior chemoimmunotherapy exposure, and age. TP53 aberration was associated with inferior TTNMD[cBTKi+BCL2i] regardless of treatment sequence (HR 3.15, p=0.0006).
For those who received cBTKi->BCL2i, the median TTNMD[cBTKi] was 39.5 months, and median TTNMD[BCL2i] was 44.5 months. For those who received BCL2i->cBTKi, median TTNMD[cBTKi] was 22.4 months, and median TTNMD[BCL2i] was not reached. OS at 60 months was estimated at87% for cBTKi->BCL2i and 75% for BCL2i->cBTKi (p=0.09).
Conclusion:
For patients who received sequential novel agents, either cBTKi->BCL2i or BCL2i->cBTKi, the overall duration of disease control achieved with these two classes of agents was not significantly different regardless of sequence. Future multicenter collaborations may allow for greater power to detect differences between these sequences. These data support basing treatment decisions on patient preference and comorbidities for patients with CLL when selecting between cBTKi and BCL2i as the first novel agent-based therapy.
Keywords : Chronic Lymphocytic Leukemia, Novel Agents, Sequencing
Please indicate how this research was funded. : This research was not funded.
Please indicate the name of the funding organization.: No funding source.